T3 therapy is a key concept of the Scorch Protocol, even when all blood markers and temperature are normal. It is required when the temperature is below normal.
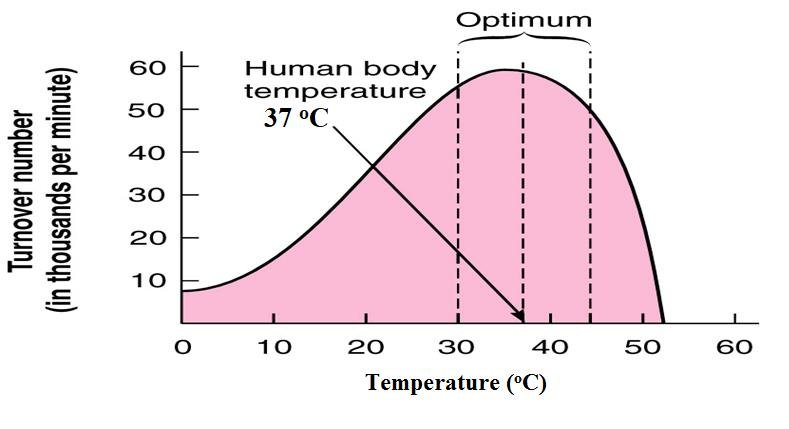
Q1: How can a low body temperature cause so many different symptoms? Nearly all chemical reactions in the body are catalyzed by enzymes, which are proteins that depend on their precise shape for activity. Low body temperature makes enzymes too tight, too slow, reducing their function and leading to a wide variety of symptoms like fatigue, brain fog, headaches, and weight gain. Body temperature correlates best with symptoms, even when thyroid labs are normal.
Q2: How is body temperature measured during T3 therapy, and why is it important? Measure orally with a mercury or accurate digital thermometer for 5-10 minutes, three times daily: upon waking (before rising), mid-afternoon (2-4 PM), and before bed. Average them—aim for 98.6°F. Daytime temps (when they should peak) reveal issues; low patterns (below 98.2°F average) indicate sluggish metabolism despite normal labs.
Q3: How low does my temperature have to be to indicate a problem with T3 utilization? Temps consistently below 98.2°F average (e.g., 97.1-97.4°F as measured in the office) are low enough to explain symptoms. Afternoon temps around 96.4°F strongly suggest a problem with T3 utilization. Track for 3-5 days for a pattern.
Q4: Do I need all the classic hypothyroid symptoms to have Wilson's temperature syndrome? No, one symptom like fatigue or cold intolerance can suffice if tied to low temps. Symptoms vary; low temperatures affect people differently, causing issues from migraines to edema.
Q5: Can WTS explain why I'm still symptomatic on thyroid meds like Synthroid? Yes, normal labs (TSH/T4) don't reflect cellular T3 delivery. WTS involves poor T4-to-T3 conversion under stress, leading to cellular starvation. T4 meds may not raise temps/symptoms; T3 resets this.
And then there are some people who stay on only T3 forever. If you want to read some T3-only life-long protocols, check out Paul Robinson's Circadian T3 Method.
Q6: Is low temperature the same as hypothyroidism? Not always, it is a functional issue (reversible with T3), while hypothyroidism is glandular damage. Both show low temps/symptoms, but WTS responds to short T3 cycles without lifelong meds.
Q7: What tests should I request from my doctor for suspected T3 problems? Full thyroid panel (TSH, free T4, free T3, reverse T3), CBC, cortisol/DHEA, ANA, EKG. But focus on temp logs and symptoms; labs are often normal in chronic fatigue syndrome.
Q8: Can WTS cause high cholesterol, and does treatment lower it? Yes, low temps slow metabolism, raising cholesterol. WT3 often drops it dramatically (e.g., 100+ points). Monitor with liver/cholesterol panel.
Q9: Are symptoms like PMS or migraines linked to low body temperature? Yes, low temps disrupt hormone balance and enzyme function, worsening PMS, migraines, or fluid retention. Many report 80-100% relief at 98.6°F.
Q10: Can kids or teens have WTS? Yes, symptoms like night sweats, low temps (95.5°F), fatigue, and allergies in a 6-year-old could indicate it. Track temps; consult pediatrician for tests/T3 trial. I would personally start extensive tests to rule out any other co-issues. Still, chronic illness with a low temperature would warrant trying some form of low-dose Armor Thyroid (NDT - Natural Desiccated Thyroid) and seeing if symptoms improve.

