I've added my own sub-notes throughout the article in the form of these callout boxes. Most of this information is based on Ray Peat's work.
The Scorch Protocol approach to chronic illness is very low-carb eating that transitions into a long dry fast, followed by a focus on glucose oxidation.
If you want a personal question answered, go to the dryfastingclub forums and leave it there. https://forums.dryfastingclub.com
If you fix glucose oxidation, you can eat 200–700 g of carbs per day and get calmer, leaner, stronger, with better sleep, higher T3, DHEA-S, IGF-1, and lower cortisol, all without the low-carb crash.
- You don’t have a carb problem, you have an oxidation problem. Your PDH is blocked, fatty-acid oxidation (FAO) is dominating, and your redox balance is stuck.
- Low-carb “works” … by raising stress hormones and avoiding the real issue. It’s a patch, not a cure. When someone adds carbs back in, they’re still insulin resistant, showing they never solved the problem.
- Add carbs on top of that broken system and you get bloat, fatigue, blood sugar spikes, then you blame the carbs instead of your metabolism.
For the last decade, I’ve experimented with everything from high-carb (300–400 g/day) to very low-carb (0–10 g/day) and everything in between.
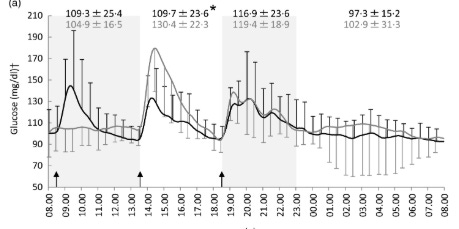
Right now, I’m eating 700 g of carbs per day for my 20-banana-a-day experiment and my blood sugar is spectacular.
My fasting glucose sits between 70–80 mg/dL, and even after massive carb meals, it rarely exceeds 120–140 mg/dL, often staying under 100 mg/dL.
My fasting insulin and C-peptide are on the lower end of normal, showing superior insulin sensitivity without needing 30k steps a day, HIIT before every meal, or metformin.
My last HbA1c was 4.9.
Carbs aren’t bad. Poor oxidation is.
Next, we’ll break down why people think carbs are the problem, how poor glucose oxidation sabotages hormones, and how to rebuild your metabolism so carbs start working for you again.
Why This Matters
When you oxidize glucose properly, you get:
- Higher thyroid output (T3) → faster metabolism, more energy, better mood.
- Higher DHEA-S & free testosterone → more drive, focus, confidence, libido.
- Higher IGF-1 → faster recovery, muscle growth, better skin and hair.
- Lower cortisol & adrenaline → calmer mind, better sleep, deeper recovery.
In short:
Proper glucose oxidation is what flips you from stressed survival mode to anabolic, high-performing mode.
That’s what this guide is about, not how to eat more carbs, but how to burn them cleanly again.
The Basics: What Happens When You Eat Carbs
Most people think “carbs = sugar = insulin spike,” but what actually happens inside your body is a beautifully coordinated energy delivery system. Here’s how it works step by step:
1. Digestion & Absorption
- Glucose and fructose are broken down from starches and sugars (fruit, milk, etc.) in the small intestine.
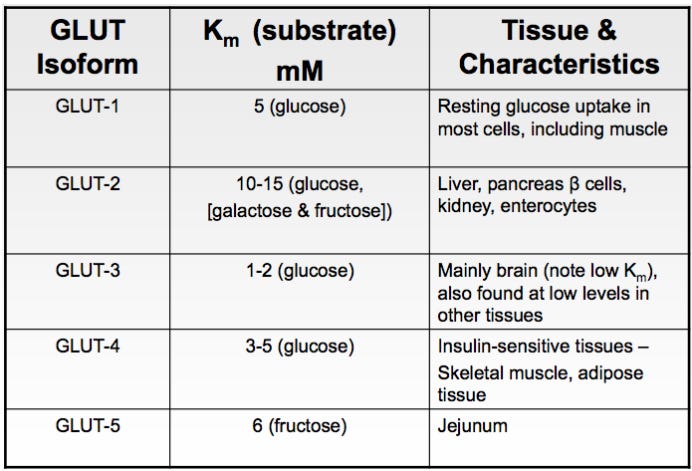
- They’re absorbed through specialized transporters:
- SGLT1 and GLUT2 move glucose (and galactose) across the intestinal lining.
- GLUT5 moves fructose in.
- Fructose absorption is slower, which helps smooth blood sugar spikes.
- Most of the eaten fructose is converted to glucose inside the intestinal wall before it even reaches the liver.
2. First Stop — The Liver
- The absorbed sugars flow directly to the liver through the portal vein.
- The liver acts as a glucose buffer, it decides how much to store and how much to release.
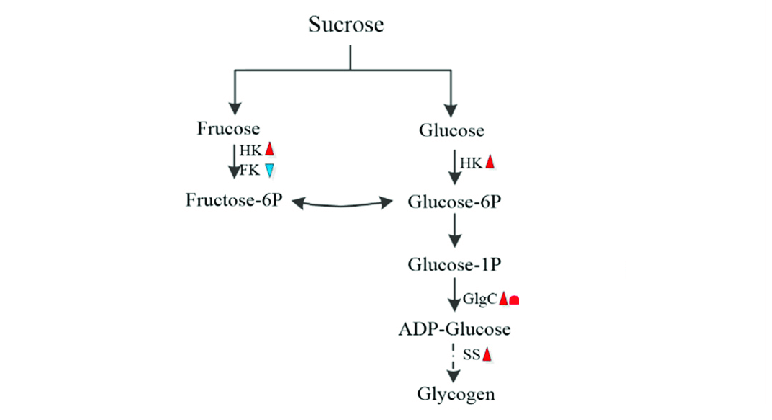
- Fructose is mostly handled here; it’s quickly turned into glycogen or glucose, making it the best fuel for refilling liver glycogen.
- Glucose is partly stored as liver glycogen, regulated by the enzyme GSK-3β (glycogen synthase kinase-3β; being inhibitory).
- When insulin is released from the pancreas, it suppresses GSK-3β, activating glycogen synthase, letting the liver store glucose efficiently.
- There are diabetic drugs that inhibit GSK-3β to help lowering circulating glucose and improve insulin sensitivity.
3. Into the Bloodstream & Tissues
- The liver releases glucose into circulation.
- Insulin tells muscle, fat, and other tissues to take up that glucose via GLUT4 transporters. Glucose can be passively taken up without insulin via the GLUT1 transporter.
- Fructose can slip into cells independently of insulin through GLUT5, and interestingly, it can enhance glucose uptake (insulin memetic effect); one reason fruit before starch lowers the glycemic response of a meal.
4. Inside the Cell — Storage or Burning
Once glucose is inside, it has two main fates:
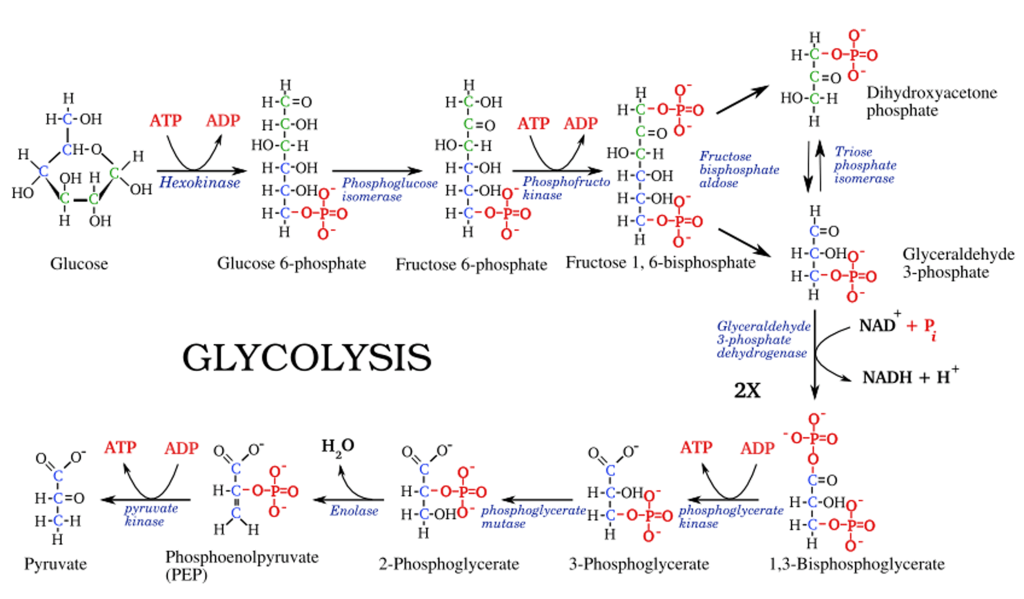
- Glycolysis yields small amounts of ATP and NADH, but the real energy comes later.
Burned immediately through glycolysis — a 10-step pathway converting glucose → pyruvate.
Stored as glycogen for later use.
5. The Mitochondrial Gate — Pyruvate Dehydrogenase (PDH)
Pyruvate now has two options:
- PDH is the key “gatekeeper” of glucose oxidation, it decides whether carbs are burned or fermented (converted to lactate).
- PDH activity is limited by:
- High NADH/NAD⁺ ratio (redox imbalance)
- High ATP (already plenty of energy)
Fatty acid oxidation (Randle cycle inhibition)
Or, if PDH is inhibited, it’s reduced to lactate instead, recycling NADH back into NAD.
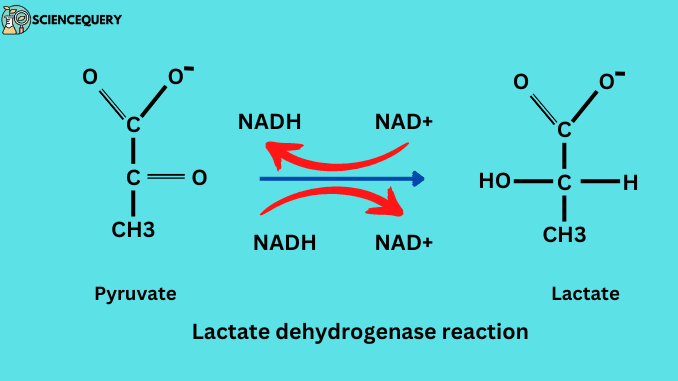
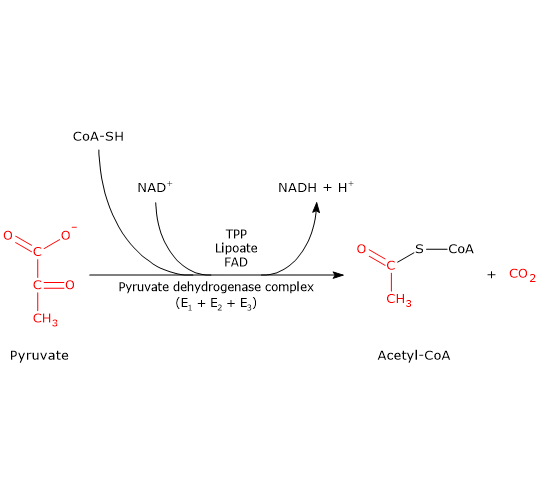
Enter the mitochondria and be converted to acetyl-CoA by pyruvate dehydrogenase (PDH).
When PDH is sluggish, lactate builds up, a sign that glucose is entering the cell but not reaching the mitochondria.
6. The Krebs Cycle (TCA Cycle)
- Inside the mitochondria, acetyl-CoA joins with oxaloacetate to begin the Krebs cycle.
- These high-energy carriers then feed electrons into the electron transport chain (ETC).
Each turn strips hydrogens and electrons, loading them onto NAD⁺ → NADH and FAD → FADH₂.
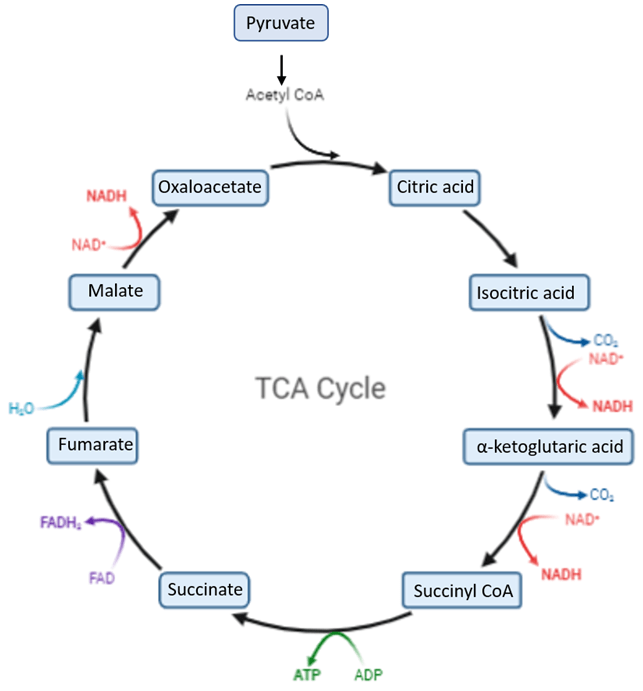
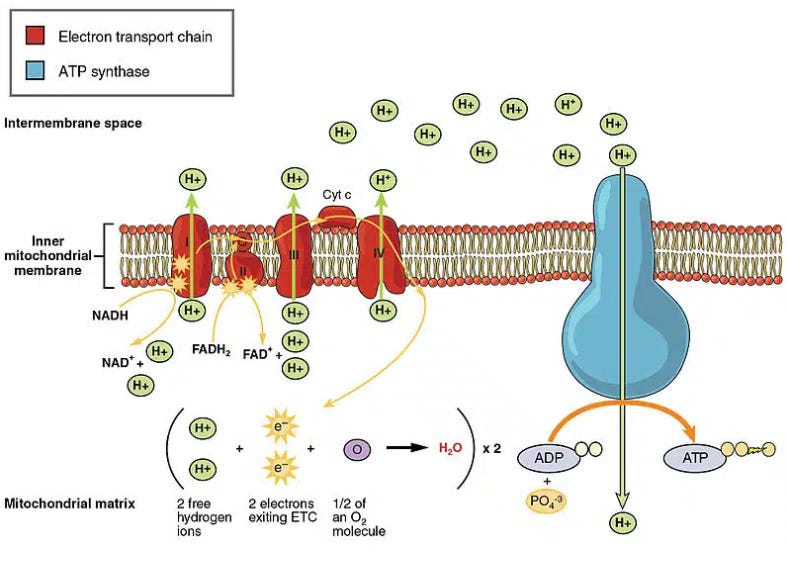
7. The Electron Transport Chain (ETC) — Energy Factory
- NADH and FADH₂ deliver electrons to CoQ10 (ubiquinone), then down the chain of complexes (I → III → IV).
- This flow drives proton pumps that create a gradient across the inner mitochondrial membrane.
- The enzyme ATP synthase (Complex V) uses that gradient to make ATP — the universal energy currency of your cells.
- As electrons reach the end, they combine with oxygen to form water, while CO₂ is produced earlier in the Krebs cycle, together signaling efficient oxidation.
8. When Everything Works Right
- Glucose and fructose flow smoothly from food → blood → cells → mitochondria → ATP.
- CO₂ rises, oxygen is efficiently used, lactate stays low.
- The result? Steady energy, warm body temperature, calm nervous system, and strong anabolic hormones.
9. When Things Go Wrong
- Glucose or fructose isn’t properly absorbed in the gut, which leads to fermentation and SIBO like symptoms such as bloating and gas.
- In the liver, glycogen isn’t properly formed, leading to high circulating glucose.
- Insulin release is insufficient, leading to high blood sugar.
- If PDH is inhibited or the redox balance is off:
- Pyruvate piles up → lactate ↑ (even if fasting glucose is normal)
- Mitochondria underperform → ATP ↓
- Stress hormones rise to compensate → cortisol ↑, adrenaline ↑
- The body feels the drop in energy and blames the carbs, when the real issue is oxidation, not intake.
Why People Think Carbs Are the Enemy
Let’s start with what goes wrong.
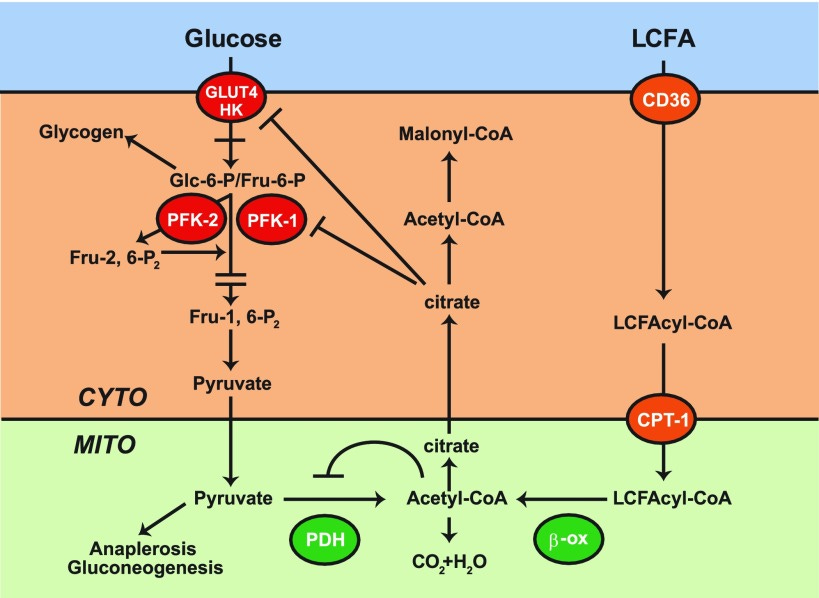
Most people don’t oxidize glucose well because their PDH enzyme is blocked and their metabolism is dominated by fatty acid oxidation (FAO).
That’s the Randle Cycle in action, the metabolic tug-of-war between fats and carbs for mitochondrial entry.
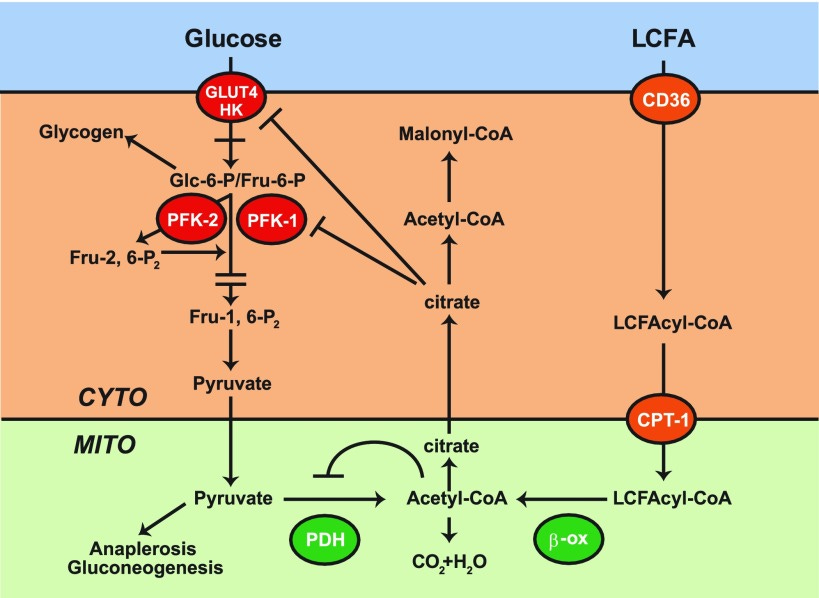
When fats win, glucose loses.
- High free fatty acids flood the blood (from stress, fasting (even an overnight “fast”), low-carb, or inflammation).
- Those FFAs inhibit glucose uptake into a cell (leading to hyperglycemia) and pyruvate dehydrogenase (PDH), the enzyme that lets glucose enter the mitochondria.
- Result: glucose isn’t taken up and can’t be oxidized → builds up as lactate → fatigue, brain fog, poor recovery.
The body sees this and panics.
It pumps out cortisol, adrenaline, and glucagon to mobilize even more fat and sugar, creating a stress loop where fat oxidation keeps glucose blocked, and glucose builds up without being used.
This is why people feel “stable” on low-carb: they stop feeding the broken system.
But they’re doing it by raising stress hormones and lowering metabolism, not by fixing the underlying issue.
What This Looks Like in Real Life
- You feel energetic but “wired.”
- You sleep poorly, wake up hot or anxious at 3 a.m (mostly due to hypoglycemia; this happened to me all the time when my metabolism was broken)
- You lose muscle fullness and pump.
- Libido drops, SHBG rises.
- Labs show high fasting glucose, high HbA1c, but “normal” insulin.
- T3 drops, reverse T3 climbs, and cortisol stays elevated.
Interestingly, the patients who seem to be the most predisposed towards developing Wilson’s Temperature Syndrome (earlier in life with less provocation) seem to predominantly belong to certain nationalities such as, Scotch, Irish, Welsh, American Indian and Russian (as well as from other countries which have been plagued with famine). Read more here.
That’s not “fat-adapted.”
That’s stressed adaptation.
Your body has switched from running on clean, oxidative energy (glucose → CO₂ + ATP) to running on emergency mode (fatty acids → incomplete oxidation + adrenaline support).
Low-carb works the same way caffeine does: it stimulates, not heals.
As a disclaimer, burning fat isn’t bad. But avoiding glucose because glucose oxidation is broken isn’t the solution.
Why You Want Glucose Oxidation Back
When glucose oxidation is restored, everything changes.
Hormonal Upgrades
- T3 increases → Glucose promotes the conversion of T4 into T3, the thyroid’s active hormone that sets your cellular metabolism.
- DHEA-S and testosterone rise → cortisol goes down, and DHEA flows toward androgens instead of stress steroids.
- IGF-1 increases → better muscle synthesis, recovery, and youth hormones.
- Lower SHBG → more free testosterone availability.
All of this depends on glucose actually reaching the mitochondria and being burned cleanly.
Metabolic Calm
Proper glucose oxidation = high CO₂.
High CO₂ = better oxygen delivery (Bohr effect).
This means: calmer mind, better focus, lower anxiety, deeper sleep.
When oxidation is high, the nervous system finally relaxes. You don’t need caffeine or adrenaline to function.
Physical Performance
When you oxidize carbs properly:
- Muscles stay full and strong.
- Lactate drops → faster recovery.
- Energy feels smooth and powerful instead of spiky.
This is why athletes with efficient glucose oxidation can perform at high workloads on high-carb diets, while others crash trying.
Why Glucose Oxidation Fails
If carbs aren’t the problem… then why do so many people feel worse when they eat them?
Because their metabolic engine is jammed.
The problem isn’t glucose, it’s the pathway that burns it.
When glucose enters the cell, it’s supposed to flow cleanly through glycolysis → pyruvate → pyruvate dehydrogenase (PDH) → mitochondria → CO₂ + ATP.
That’s efficient oxidation. That’s how carbs raise T3, DHEA-S, IGF-1, and drive high energy metabolism.
But when oxidation breaks, that flow stalls. Glucose builds up, gets converted to lactate, insulin spikes, energy crashes, and people blame the carbs.
Here’s what’s really blocking that pathway.
1. Fatty Acid Oxidation Dominance (Randle Cycle)
When fatty acids are being burned at high rates, glucose can’t enter oxidation (this heavily depends on total caloric intake as well).
This is called the Randle Cycle, fats and carbs compete for the same mitochondrial machinery.
- High free fatty acids (FFAs) from stress, fasting, or low-carb diets inhibit PDH, the enzyme that allows pyruvate to enter the mitochondria.
- PDH inhibition means glucose can’t be oxidized, it just gets recycled into lactate.
- That excess lactate causes fatigue, brain fog, and reactive hypoglycemia after carb meals.
So when people eat carbs while FAO is dominant, they experience “carb crashes”, not because of carbs, but because fats are blocking their oxidation.
This is why suppressing fatty acid oxidation (with compounds like Pyrucet, aspirin, or meldonium) can instantly make carbs feel clean again.
2. PDH Inhibition
PDH (pyruvate dehydrogenase) is the gatekeeper between glycolysis and the mitochondria.
PDH is often shut down by stress or nutrient deficiencies:
- Acetyl-CoA excess, high ATP, high NADH to NAD, cortisol, glucagon, and adrenaline increase PDK activity.
Thyroid suppression, low B1, Mg, B2, B3, B5, or ALA deficiency make it worse. In this graph you can see all the nutrients needed and that PDH is quite a complex enzyme complex.
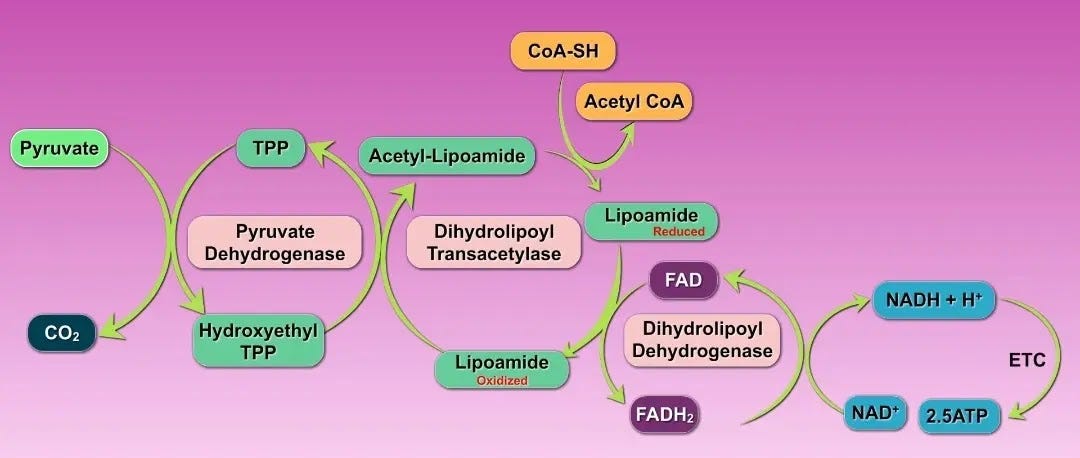
PDK (pyruvate dehydrogenase kinase) phosphorylates and inactivates PDH.

That’s why high-carb diets can only work if PDH is active.
3. Reductive Stress and Low NAD⁺
Even if PDH is open, oxidation still fails if the cell can’t recycle NADH back to NAD⁺.
That’s called redox imbalance, and it’s what traps metabolism in a pseudo-hypoxic, low-energy state.
Low NAD⁺ =
- Poor electron transport chain (ETC) function
- High lactate and ROS
- Sluggish ATP generation
- “Tired but wired” energy
Compounds like niacinamide, PQQ, and Pyrucet restore NAD⁺ and push the redox ratio back toward oxidation.
This is also why chronic stress, hypoxia, or inflammation keep you stuck in low oxidation, they drain NAD⁺ and choke mitochondrial flow.
4. Mitochondrial Dysfunction (ETC Bottleneck)
Even with glucose inside the mitochondria, oxidation depends on electron transport chain efficiency.
When Complex I or III slow down, NADH accumulates and electrons leak, creating oxidative stress instead of energy. This increases the demand for antioxidant pathways like superoxide dismutase, hydrogen peroxide and glutathione peroxidase, which is supported by zinc, magnesium, copper, selenium and manganese.
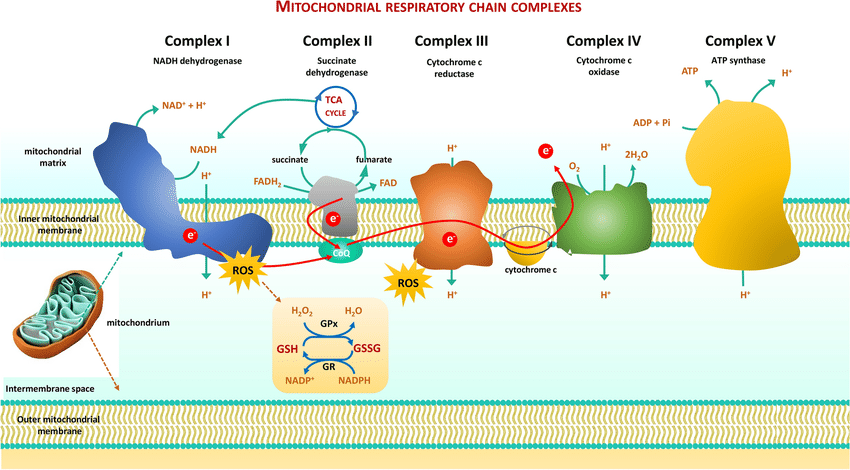
That’s why oxidative support (vitamin K2, methylene blue, CoQ10, succinate, vitamin C) can drastically increase ATP and CO₂ production.
More CO₂ = better oxygenation = calmer nervous system and deeper recovery.
The takeaway:
You can’t just eat more carbs.
You need a clean electron flow — from glucose → PDH → TCA → ETC → CO₂.
5. Gut & Endotoxin Interference
Finally, one of the most overlooked brakes on glucose oxidation is the gut.
Endotoxin (LPS) from bacterial overgrowth or poor bile flow directly inhibits PDH and activates FAO, pushing you right back into the Randle trap.
This is why people think they’re “carb intolerant.”
They’re not, they just have a gut-derived metabolic block.
Fixing digestion (improving bile flow, lowering endotoxin, reducing fermentation) can make previously “intolerant” carbs feel fine again.
The Bottom Line
You can’t burn carbs efficiently if:
- Fatty acids dominate (FAO > glucose oxidation)
- PDH is inhibited or blocked by stress/nutrient deficiency
- NAD⁺ is low and redox is reduced
- Mitochondria are sluggish
- Gut endotoxin keeps you inflamed
Once you address these, carbs start working again.
The rest of the article is all about how to restore proper glucose oxidation and include solving every step. I’ll show you how to identify which step you need to work on and how to fix it. As well as a 14 day playbook on how to get the ball rolling.
The Glucose Oxidation Restoration Playbook
Now that you understand why glucose oxidation fails, let’s rebuild it…step by step.
This isn’t about eating more carbs; it’s about teaching your body to burn them cleanly again.
Step 1 — Rebuild the Food Frame
Goal: Make carbs easy to oxidize and hard to store.
- Keep dietary fat low, especially PUFA. Fat competes with glucose inside the mitochondria (Randle Cycle).
- The more carbs you want to eat, the lower your fat needs to be. If you keep fat really low, <30-40g daily, then your carb intake can be much higher since there is very little fat preventing proper glucose oxidation.
Once you dive into Ray's work, you'll realize that most of Hans' recommendations are derived from there.
- Structure meals for oxidation:
- Morning: lower-fat, protein-focused or fruit-based if your dawn response is good.
- Afternoon–Evening: heavier on starch once cortisol has dropped.
- Use fructose strategically.
- Fructose bypasses GLUT-4 dependence and helps insulin-resistant muscle cells pull in glucose.
- Getting most of your carbs from whole fruit (banana, apple, pears, oranges, etc.) will be much better than slamming fruit juice, unless you test and see your glycemic response is really good.
- Prioritize potassium & magnesium. They’re insulin cofactors; deficiency mimics insulin resistance.
- Potassium-rich: fruit, potatoes, dairy.
- Magnesium-rich: milk, banana and other fruit, cocoa.
Second meal effect: Skipping breakfast resulted in a significantly higher glycaemic response (more than double) after lunch compared to eating breakfast (R).
Keep protein nutrient-dense: milk + red meat + oysters + eggs + dairy. These supply zinc, copper, and B-vitamins that drive PDH. Higher protein intake reduces meal glycemic responses (R).
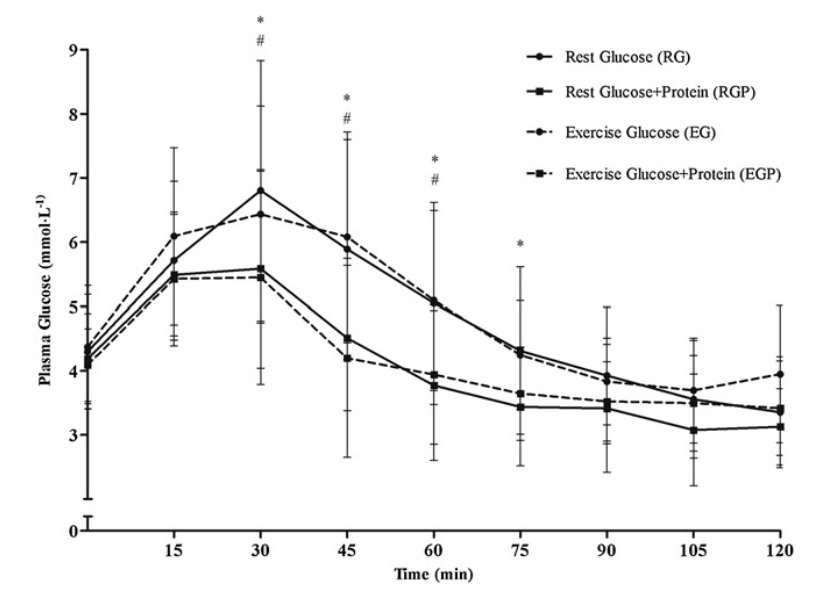
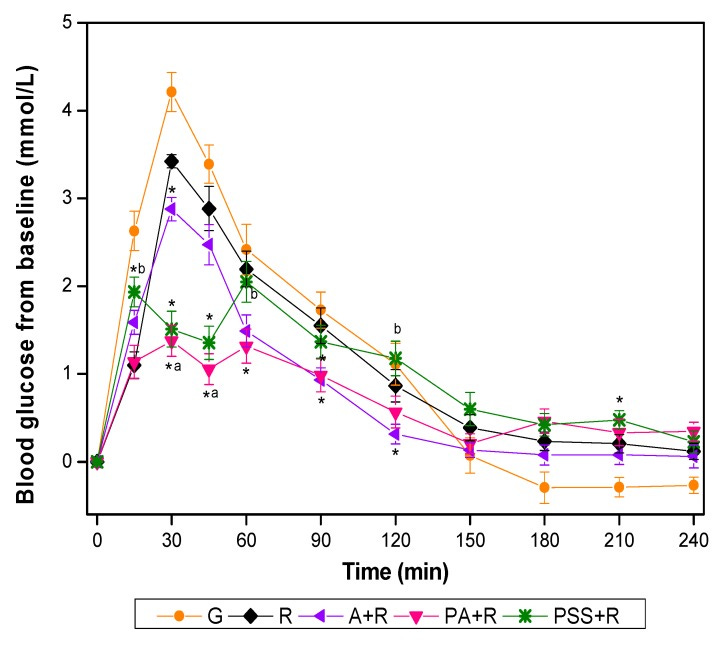
Eating an apple (pink line) or fruit juice before starch enhances glucose uptake and liver glycogen storage. Even adding sugar (green line) to your carbs can help to blunt the insulinogenic effect.
Step 2 — Lower FAO Pressure (Unblock the Randle Cycle)
Goal: Stop fats from stealing mitochondrial bandwidth.
- Aspirin (500–1000 mg/day) — blunts lipolysis, lowers FFAs, improves insulin sensitivity. Excellent for those with high fasting glucose in the mornings.
- Pyrucet (ethyl pyruvate + ethyl acetoacetate) — directly inhibits excessive FAO (~50%), activates PDH, raises NAD⁺.
- Meldonium (Mildronate) — optional; limits carnitine-dependent FAO for deeper metabolic reset.
- Very low to ultra low-fat meals + these interventions = maximal glucose flux. Think >95% lean ground beef + rice or whey + glucose powder or shimp + squid + rice. Very very lean meals with no added fat.
Morning strategy & the Dawn Effect
Cortisol and GH rise before waking, spiking FFAs and transient insulin resistance.
That’s why big carb breakfasts make some people crash, because they body has to release a lot of insulin, which can then lead to reactive hypoglycemia.
Fix it two ways:
1️⃣ Eat lower-carb / higher-protein early and push starches later.
2️⃣ Or override the dawn effect with 1 g aspirin + Pyrucet on waking — drops FFAs, activates PDH, and lets you oxidize carbs even at dawn.
I’ve used this combo for months at a time when I was hypothyroid: no crash, stable glucose, warm hands within 30 minutes.
Step 3 — Activate and Unblock PDH
Goal: Re-open the gate that lets glucose into the mitochondria.
- Unblock the enzyme:
- Carnitine (1–2 g/day) — shuttles acetyl groups and supports PDH balance.
- DCA (12.5–25 mg/kg 2–3×/wk) — powerful PDK inhibitor; use cautiously and cycle.
- Pyrucet - inhibits fatty acid oxidation and increases the NAD/NADH ratio.
- Upregulate PDH activity:
- Vitamin B1 (300–600 mg/day (even up to 2g daily if needed) — essential cofactor; fixes lactic buildup.
- Magnesium (200–400 mg/day) — stabilizes enzyme activity.
- B2, B3, B5 + ALA — coenzymes for PDH & TCA.
- Adequate thyroid (T3) — naturally boosts PDH and mitochondrial biogenesis.
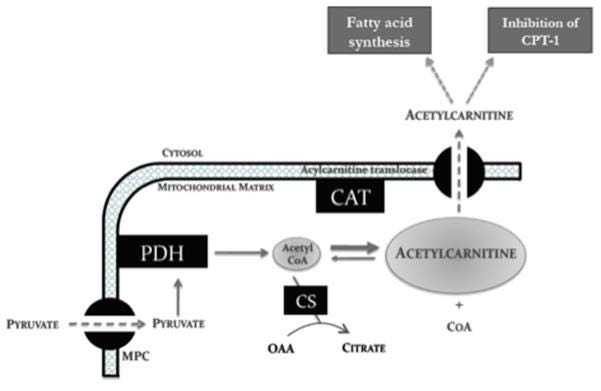
Carnitine increases PDH and subsequent CO2 production in a dose dependent manner (R).
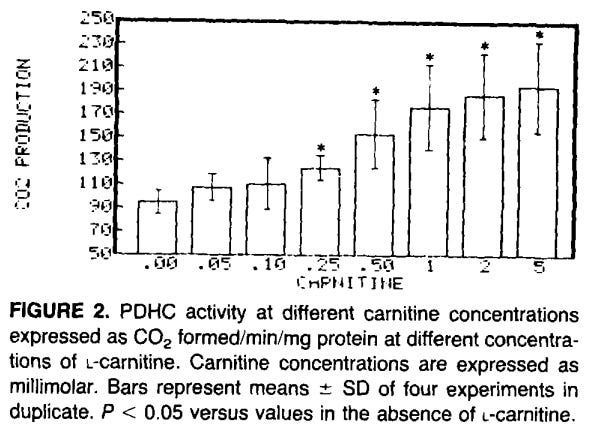
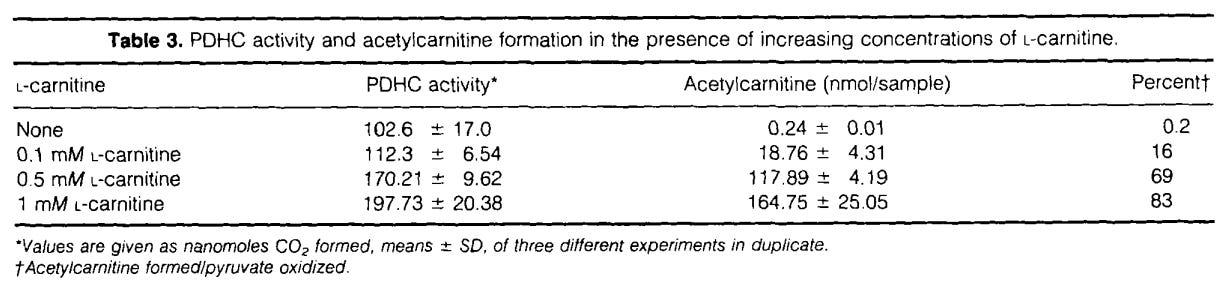
When glucose and fat are being burned, it creates acetyl-CoA, which inhibit PDH. Carnitine acetyltransferase catalyzes the conversion of acetyl-CoA to acetylcarnitine, which can be transported out of the mitochondria, thereby lowering intramitochondrial acetyl-CoA and relieving PDH inhibition (R).
Step 4 — Restore NAD⁺ & Redox Balance
Goal: Keep the electron flow moving.
- Niacinamide (250–500 mg 2×/day) — raises NAD⁺.
- PQQ (20–200 mg/day) — stimulates mitochondrial biogenesis and increases NAD/NADH ratio.
- Pyrucet — supports NAD⁺ regeneration directly.
- Optional: Methylene Blue (0.5–2 mg/kg) + Vitamin K2, CoQ10, succinate, Vitamin C to keep the ETC clear.
I think you'll do best with focusing on this core: T3, Aspirin, Slow-release methylated B complex, B1, d3+k2. Then add on only what is necessary or what you can afford. Fluconazole for 3-6 months is a blank recommendation that I give to anyone with a chronic illness.
Step 5 — Fix the Gut and Bile Flow
Goal: Remove the hidden block on PDH and thyroid.
- Endotoxin (LPS) from bacterial overgrowth inhibits PDH and raises FAO. Use 1 tsp of activated charcoal before bed to help bind to endotoxin overnight. This will help to improve insulin sensitivity the next morning if endotoxin is the problem. Here’s my full guide on how to lower endotoxin.
- Improve bile flow: taurine, glycine, bitters, or TUDCA.
- Speed transit: potassium-rich fruit, magnesium, 3-6g L-Carnitine, morinda (the one from Jing herbs works the best), 3-4 kiwi fruit, prune juice, Bifidobacterium lactis BB-12, HN019, and DN-173 010.
- Bind bile/endotoxin with activated charcoal, white button mushroom or calcium-rich dairy (it creates calcium soaps that help bind toxins).
- Re-evaluate food intolerances: “gluten sensitivity” and “starch intolerance” often stem from gut inflammation, not carbs themselves.
Step 6 — Train for Oxidation
Goal: Teach the body to choose carbs as the primary fuel again.
- Resistance + moderate cardio improves GLUT-4 activity.
- Avoid fasted HIIT or extreme glycogen depletion — both spike cortisol and FAO.
- Track biofeedback: warmth, pulse 80–90 bpm, good mood = oxidation on.
- Poor sleep, cold limbs, racing heart = FAO creeping back.
Testing & Targets: How to Know If You’re Actually Oxidizing Glucose
You can’t improve what you don’t measure.
Most people “feel” whether a diet is working, but feelings can lie.
Oxidation doesn’t.
If glucose oxidation is working, you’ll see it in your data, your energy, and your mood.
Here’s how to track it objectively.
1. Post-Meal Glucose Tracking
Keep on mind that different carbs can give you different spikes. You can go off the high GI and glycemic load charts, but at the end of the day, you’ll have to test for yourself to see how you specifically respond to specific foods.
How to test:
Take glucose readings at 15, 30, 60, 90, and 120 minutes after a carb-heavy meal.
You can use a CGM or a simple fingerstick glucometer.
Importantly, your glycemic response to the same food/meal can be different at breakfast, lunch and dinner, so test all those meals. Just 1 day is enough to see how your body responds. After that, you don’t have to track every meal, but only the specific meal/food that you’d like to improve.
Ideal pattern:
- Fasting glucose: 70–85 mg/dL
- 15 min peak: <140mg/dL. Sometimes this peak might be higher if you eat a pure carb meal, like 2 glass of apple juice on its own. However, such a short spike is not going to create glycation (increase HbA1c) or make you diabetic. It’s the prolonged elevation that’s the problem.
- 30 min peak: <140 mg/dL.
- 1-hour: <100 mg/dL
- 2-hour: back near baseline (70–85 mg/dL)
That’s a healthy oxidation curve, quick uptake, clean burn, no prolonged elevation.
If you stay above 140 mg/dL for longer than 2 hours, you’re not oxidizing efficiently.
What to do if it’s off:
- Peak too high → lower meal fat, add more lean protein, add an apple or fruit juice before starch.
- Peak too long → add PDH cofactors (B1, Mg, Pyrucet) and use a lipolysis inhibitor like aspirin.
- Post-meal dip or fatigue → check thyroid markers, or too much FAO from stress/fasting. This is also usually a sign of excess lipolysis and can be solved with aspirin and a higher protein meal.
2. Morning and Evening Metrics
Body Temperature:
- Morning: 36.8-37.1°C (98.2-98.8°F)
- Midday: 37-38°C (>98.6°F)
Low temps suggest sluggish oxidation or low thyroid.
Pulse:
- Morning: 60–80 bpm
- Midday: 70–90 bpm
A steady, warm pulse = active PDH and mitochondrial flow.
Cold hands, low pulse, and fatigue = fat oxidation dominance.
3. Subjective Markers (The Human Metrics)
You’ll know oxidation is back when you:
- Feel warm most of the day, not cold or anxious.
- Have stable energy — no post-meal crash or need for caffeine.
- Sleep deeper, wake refreshed.
- Recover faster from workouts.
- Notice higher libido, calm confidence, and a sense of “clean energy” instead of wired stimulation.
Those are signs of high CO₂ production — the hallmark of glucose oxidation.
4. Optional Lab Tracking
If you like data (like me), here are the main blood markers that confirm your glucose oxidation is actually working:
- Fasting Glucose (70–85 mg/dL) — reflects low stress hormones and efficient glucose uptake.
- HbA1c (4.7–5.3%) — shows long-term glucose control without chronic elevation.
- Fasting Insulin (2–5 µIU/mL) — low insulin requirement = high sensitivity.
- C-Peptide (marker of 24 hour insulin release; low-normal range) — indicates efficient insulin production and utilization.
- Triglycerides — <150. When glucose is converted to fat instead of being burned, it shows poor glucose oxidation.
- Free T3 (upper-normal) — drives PDH activity and overall oxidation rate.
- Cortisol (AM moderate range) — not chronically high; means the body isn’t relying on stress hormones to maintain blood sugar.
- SHBG (low-normal) — signals proper androgen status and low cortisol.
- DHEA-S / Testosterone / IGF-1 (high-normal) — reflects restored anabolic drive and metabolic efficiency.
- Lactate (low-normal; <1 fasting) — low lactate = efficient oxidative metabolism.
- Ferritin, hsCRP, ESR, ALT, AST, bilirubin, GGT (normal-low) — clean liver metabolism and low inflammation.
5. Combine Glucose Data with Context
If you’re using CGM, don’t obsess over every spike.
A short spike with fast recovery means a healthy insulin response.
Flatlines mean cortisol dominance or poor insulin signaling.
I prefer dynamic data over static fasting values.
The way your glucose moves after a meal tells you more about your metabolism than your fasting number ever will.
6. The Weekly Review Routine
Every 7 days, ask yourself:
- Are my hands and feet warm?
- Is my energy smooth throughout the day?
- Did I wake up rested?
- Are my workouts stronger?
- Is my glucose returning to baseline faster?
If 3 or more are true — your glucose oxidation is improving.
If not, go back and check:
- Fat too high?
- Missing B1, Mg, or PQQ?
- FAO not suppressed enough (add Pyrucet or aspirin timing)?
- Gut symptoms still blocking progress?
7. The Endgame Metric — CO₂ and Calm
When oxidation is restored, you don’t need external stimulants to function.
You’ll notice it: your breathing slows, your thoughts quiet, and your drive increases.
That’s CO₂ doing its job — oxygenating your tissues, balancing your nervous system, and turning carbs into clean ATP.
That’s when you know you’ve crossed from “managing blood sugar” → to mastering metabolism.
Protocols by Carb Level
Not everyone needs 700 g of carbs to restore oxidation.
Some people thrive at 200 g; others, like me right now, can burn 700 g daily without a single spike.
The difference isn’t genetics, it’s how efficient your oxidation system is.
Below are two frameworks you can plug into depending on where you’re at in your metabolic recovery.
Protocol A — The 200 g/day Oxidation Reset
Goal:
Restore oxidation without forcing high-carb intake too soon. Ideal for those coming from low-carb, keto, or with signs of poor insulin sensitivity.
Macro & Food Setup
- 150–200 g carbs daily from ripe fruit, juice, potatoes, or white rice.
- Keep fats low-moderate (50–70 g) and protein high-quality (1.2–1.6 g/kg).
- Emphasize potassium-rich and magnesium-rich foods to improve insulin signaling.
- Pair starches with fruit or juice (e.g., apple before rice) to smooth post-meal glucose curves.
Supplement & Stack Setup
Most often, simple dietary changes will be enough and you don’t need supplements, but the right supplements can help to fast-track your progress.
- B1 (300 mg) + Mg (200–400 mg) daily — PDH activation.
- Niacinamide (250–500 mg twice daily) — raises NAD⁺, lowers FAO.
- Pyrucet (start with low dose) — suppress FAO, enhance PDH flux.
- Aspirin (325–1000 mg daily once a day or with each meal if needed) — reduces lipolysis, supports insulin sensitivity.
- Optional: small dose of PQQ or ALA for redox and mitochondrial support.
Training & Lifestyle
- Light resistance training 3–4x/week to activate GLUT-4 and burn glucose.
- Avoid fasted workouts — they reinforce FAO.
- Morning: lower-carb, higher-protein meals (unless using aspirin + Pyrucet).
- Track post-meal glucose at least once a day for feedback.
Expected Benefits
- Warmer hands and feet.
- Lower fasting glucose within 2 weeks.
- Improved sleep, mood, and libido.
- Reduction in cortisol and SHBG, rise in T3 and DHEA-S.
You’ll know you’re ready to move up when you can handle 200 g/day with glucose peaking <130 mg/dL and energy feeling smooth all day.
Protocol B — The 700 g/day High-Flux System (Advanced)
Goal:
Maximize oxidation capacity, glycogen storage, and anabolic drive.
This level is for people with strong metabolic flexibility, regular training, and low stress markers.
Macro & Food Setup
- 600–750 g carbs daily — fruit, juice, potatoes, white rice, honey, and milk.
- Keep fat very low (under 40–50 g).
- Protein steady at ~1.5 g/kg, focusing on lean red meat, seafood like squid, oysters, shrimp, eggs, low fat dairy, and collagen.
- Split carbs evenly through 4–6 meals.
- Eat fruit or juice before starch to maintain glucose stability and fill liver glycogen first.
Supplement & Stack Setup
Again, keep in mind that these supplements aren’t needed if your glucose oxidation is on point. But very often, people have a deficiency, which results in much higher glucose spikes, thus people blaming carbs. Once you’ve fixed those deficiencies, you won’t need supplements anymore just to burning glucose the way you should.
- Pyrucet (6–10 mg/kg/day) split between meals — keeps FAO suppressed and PDH activated.
- Aspirin (500–1000 mg in the morning) — limits lipolysis, prevents dawn-effect resistance.
- B1 (600 mg/day) + Mg (400 mg/day) + B2/B3/B5 — strong PDH/TCA activation.
- Niacinamide (500 mg 2×/day) — raises NAD⁺ and redox potential.
- PQQ (20-200 mg) + Vitamin K2 or CoQ10 — ETC support for high oxidative throughput.
- Potassium & sodium balance: 3–4 g K, 4–5 g Na daily for glycogen hydration and performance.
Training & Lifestyle
- Resistance training or mixed anaerobic sessions 4–6×/week.
- Add 1–2 steady-state cardio sessions for glycogen turnover and insulin sensitivity.
- Avoid long fasts. Burning fat isn’t a problem, but going many days/weeks without eat much carbs can results in impaired glucose oxidation, as we see in people who do carnivore or keto.
- Use aspirin + Pyrucet in the morning to flatten the dawn cortisol/FFA surge.
Expected Benefits
- Consistent warmth and calm focus all day.
- Stable glucose (70–85 mg/dL fasting, <120 post-meal).
- Drastic improvement in thyroid output, testosterone, and IGF-1.
- Deep, uninterrupted sleep and high recovery capacity.
- Pumped muscles and steady endurance — zero reactive dips.
Amino Acid Support for Glucose Oxidation
Two simple amino acids, glycine and taurine, have consistent human and animal data showing they enhance insulin sensitivity and flatten glucose spikes. They complement every carb protocol by improving the body’s ability to oxidize glucose instead of storing it.
Glycine
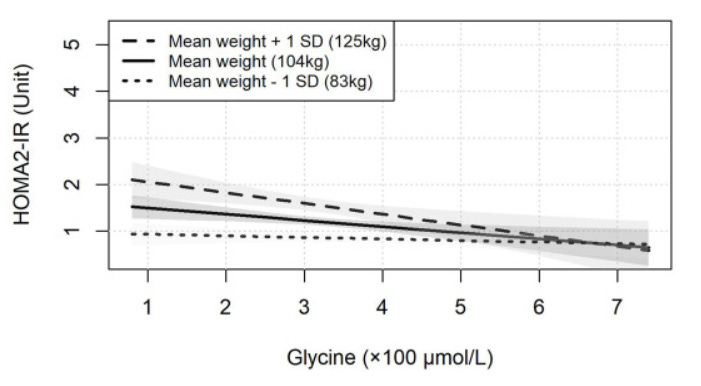
- Human pilot study (2014) — 4 weeks of glycine improved insulin sensitivity and glucose tolerance in insulin-resistant subjects (R).
- Animal study (El-Hafidi 2018) — Glycine reversed sucrose-induced insulin resistance and boosted glutathione synthesis (R).
Population data — Low serum glycine correlates with insulin resistance and diabetes risk (R).
Taurine
- Meta-analysis (2022, Tao et al.) — Reduced fasting glucose and HbA1c (R).
- Mechanistic review (2010, C de la Puerta) — Taurine improved β-cell function, hepatic insulin action, and glucose tolerance (R).
- RCT (2024, Sun et al.) — Long-term taurine supplementation was particularly effective for obesity-related insulin resistance (R).
Why they fit the oxidation model
- Both raise cellular NAD⁺/redox efficiency, increase glutathione, and enhance PDH flux indirectly.
- Combined with Pyrucet or a high-carb meal, they help push glucose toward full oxidation instead of partial glycolysis/lactate production.
Typical use
- Glycine 3–5 g pre-meal or before bed (calms CNS and blunts post-meal glucose).
- Taurine 1–3 g/day, split across meals (e.g. 2g per big meal; synergistic with magnesium and niacinamide).
The Stack & Dosing Blueprint
By now, you understand the theory: carbs aren’t the problem, poor oxidation is.
Here’s the practical part: the exact stacks, dosages, and timing that restore oxidation and keep it running 24/7.
These compounds aren’t magic, they simply remove the metabolic brakes your body has been stuck under.
1. Fatty Acid Oxidation & Lipolysis Control
Goal: Stop excess fat oxidation from hijacking the mitochondria.
- Aspirin — 325–1000 mg/day or per meal if needed. In many studies, the researches gave diabetic patients 4g of aspirin a day to improve insulin sensitivity. There is even a study where they gave type 1 diabetic men 8-9g of aspirin a day and 2 men were able to completely stop their insulin shots.
- Inhibits lipolysis and lowers FFAs.
- Enhances insulin sensitivity and reduces inflammation.
- Best timing: morning, 30 minutes before your first carb meal (or upon waking) or with your first meal.
- Combine with vitamin K2 (1–5 mg) if used daily long-term to maintain clotting balance. I don’t do this, but some people bleed much easier and will need this.
- Pyrucet — 6–10 mg/kg/day
- The centerpiece of the protocol.
- Ethyl pyruvate + ethyl acetoacetate directly inhibit excessive FAO (~50%) and activate PDH.
- Improves NAD⁺/NADH ratio, lowers lactate, and enhances redox state.
- Best timing: split around carb meals (e.g., ⅓ breakfast, ⅓ lunch, ⅓ pre-training).
- Stacks beautifully with aspirin and niacinamide for full Randle Cycle suppression.
- Meldonium (optional, 250–500 mg 2×/day)
- Inhibits carnitine synthesis and FAO at a deeper level.
- Use if coming from low-carb or high-FFA states, but cycle (2–3 weeks on, 1–2 off).
2. PDH Activation Stack
Goal: Reopen glucose’s gateway into the mitochondria.
- Vitamin B1 (Thiamine HCl or Benfotiamine) — 300–600 mg/day
- Cofactor for PDH, alpha-ketoglutarate dehydrogenase, and transketolase.
- High doses rapidly lower lactate and improve carb tolerance.
- Magnesium — 200–400 mg/day
- Required for every ATP-dependent enzymatic step in glycolysis and PDH.
- Citrate, glycinate, or malate forms preferred.
- B2 (20–50 mg), B3 (250–500 mg), B5 (500–1000 mg)
- Support TCA and electron transfer chain (ETC).
- Take with meals to aid absorption.
- Alpha-Lipoic Acid — 300–600 mg/day
- Recycles PDH cofactors and improves mitochondrial efficiency.
- Can mildly lower blood glucose; dose around carb meals for best results.
- DCA (Dichloroacetate, optional) — 12.5–25 mg/kg, 2–3×/week
- Potent PDK inhibitor, directly activates PDH.
- Use cautiously and cycle (3 weeks on, 2 weeks off).
- Pair with thiamine to prevent neuropathy.
3. NAD⁺ & Redox Enhancement
Goal: Ensure clean electron flow and oxidative capacity.
- Niacinamide — 250–500 mg, 1–2×/day
- Increases NAD⁺ and improves glucose tolerance.
- Synergistic with aspirin and Pyrucet for full Randle suppression.
- PQQ — 20-200 mg/day
- Promotes mitochondrial biogenesis and boosts redox cycling.
- Methylene Blue — 0.5–2 mg/kg/day (optional)
- Electron carrier; accepts electrons from NADH and donates to cytochrome c.
- Enhances ATP and CO₂ production, stabilizes mood.
- Vitamin K2 (5–10 mg)
- Acts as an alternative electron carrier and complements MB’s mechanism.
- CoQ10 (100–200 mg) + Succinate (500–1000 mg) + Vitamin C (1 g)
- Keep the ETC flowing and prevent oxidative stress.
4. Thyroid & Mitochondrial Support
Goal: Sustain PDH activation and prevent regression to FAO.
- Ensure adequate calories & carbs.
- Selenium (100–200 µg) — supports T4→T3 conversion.
- Zinc (15–30 mg) + Copper (1–3 mg) — balance is critical for thyroid and mitochondrial enzymes.
- Saturated fats over PUFA — reduce FAO competition.
- Optional: low-dose T3 (under medical supervision) if thyroid function is sluggish.
5. Synergy Stacks
Morning (Dawn Effect Override)
- 1 g Aspirin + dose of Pyrucet → suppress FAO + activate PDH.
- Follow with a moderate carb meal (fruit, honey, eggs, milk).
- Result: low FFAs, smooth glucose, strong oxidation start to the day.
Pre-Training (Performance Stack)
- 300 mg B1, 250 mg Niacinamide, Pyrucet dose, Mg, and a simple carb source (fruit, honey, or milk).
- Maximizes glucose oxidation and endurance while minimizing lactate buildup.
Evening (Recovery Stack; optional)
- 10–20 mg PQQ, 100–200 mg CoQ10, 1 g Vitamin C, 5 mg K2, and small carbs.
- Restores redox balance, improves sleep quality, and enhances glycogen replenishment.
6. Dosing Notes & Cycling
- Start low, scale with response.
Begin with half doses for 3–5 days, then titrate up once glucose stability improves. - Cycle high-intensity interventions.
DCA or meldonium: 3 weeks on / 2 weeks off. Pyrucet and cofactors can be used continuously. - Avoid combining all strong ETC boosters (MB, K2, CoQ10, PQQ) at high doses unless you know your tolerance, it can cause mild overstimulation.
7. Expected Timeline
Days 1–3:
Energy starts stabilizing, less “wired” feeling after carbs.
Days 4–7:
Sleep and temperature improve. Post-meal glucose flattens.
Days 8–14:
Steady warmth, calm focus, better workouts, higher libido.
Beyond 2 weeks:
T3, DHEA-S, and IGF-1 rise. Cortisol and SHBG fall.
You’ll feel like your metabolism is finally “online.”
Troubleshooting & Decision Tree
Even when you do everything right, there’s always a phase where your metabolism recalibrates.
Blood sugar might fluctuate, energy might dip, or digestion might feel off, that doesn’t mean the system isn’t working.
It just means you need to fine-tune which brake is still on.
Use this decision tree to quickly find the weak link and fix it.
1. High Glucose Spikes (150–180+ mg/dL post-meal)
Likely cause:
Fat oxidation dominance, sluggish PDH, or too much meal fat.
Fix:
- Lower fat in the next meal (especially long-chain fats).
- Increase lean protein
- Add fructose or fruit before starch (apple, orange juice).
- Take Pyrucet + aspirin 15–30 min before the meal.
- Increase B1 + magnesium (PDH activators).
- Check potassium intake — low K⁺ makes insulin signaling sluggish.
Goal: peak under 140 mg/dL, back near baseline within 2 hours.
If it’s still high, try a different carb source.
2. Slow Glucose Clearance (still high 2 hours after eating)
Likely cause:
Excess free fatty acids in the blood, poor PDH activity or low NAD⁺.
Fix:
- Keep fat as low as possible.
- Increase lean protein
- Use a higher aspirin dose (1-2g) with or just before the meal.
- Increase B1 and Pyrucet dose slightly.
- Ensure you’re not too low in thyroid (T3) or magnesium.
3. Reactive Hypoglycemia (crash after eating carbs)
Likely cause:
Overactive insulin response with poor oxidation and excess free fatty acids.
You pulled glucose into the cell, but can’t burn it efficiently.
Fix:
- Same as above.
4. Cold Hands, Fatigue, or Low Body Temp
Likely cause:
Poor oxidation, glucose going to lactate instead of CO2.
Fix:
- Increase lean protein
- Have something with more salt and fiber, still low fat
- Avoid liquid calories
- High dose aspirin + Pyrucet with or just before the meal.
- It could also be a sensitivity to the specific carb, so try a different carb source.
When oxidation is high, you’ll feel it — warmth, energy, calmness.
5. Feeling Wired or Anxious (especially after carbs)
Likely cause:
Stress hormones elevated, low CO₂, or redox imbalance.
Fix:
- Add aspirin to bring down stress hormones and lipolysis
- Increase niacinamide and B1 (both lower stress metabolism).
- Add PQQ or methylene blue for better NAD⁺ turnover.
- Deep nasal breathing post-meal (CO₂ retention increases oxygenation).
- Avoid fasting or training empty — both raise adrenaline.
You’re aiming for calm energy, not “stimulated” energy.
6. Gut Bloat or Food Intolerance
Likely cause:
Endotoxin, poor bile flow, or fermentable carbs feeding overgrowth.
Fix:
- Focus on very easy to digest foods - shakes, broths, etc.
- Try low FODMAP foods only
- Avoid any potential food that might cause an allergic reaction
- Speed up transit with ripe fruit, potassium, dairy, or cooked/peeled foods.
- Improve bile flow: taurine, glycine, TUDCA, or bitters.
- Bind endotoxin with charcoal, white button mushroom, or low-fat dairy.
- Rotate fruit sources; some have mild allergens (mango, kiwi, apple peel, etc.).
Don’t blame the carb, fix the digestion.
7. Poor Sleep or Night Waking
Likely cause:
Low glycogen, high cortisol/adrenaline overnight.
Fix:
- Increase protein intake.
- Increase fat intake slightly
- Take aspirin. This usually helped prevent me from waking up around 3am.
- Eat carbs + protein + salt before bed (milk, honey, or banana + gelatin). Some people sleep really well when that have a little ice cream before bed, but this is not something I advocate for. You can try it, but make sure you don’t overeat calories.
- Use Pyrucet in the evening to enhance nighttime oxidation.
- Avoid long fasting gaps before bed.
- Track heart rate during sleep, elevated HR = stress metabolism.
8. Low Motivation, Libido, or Mood
Likely cause:
Still stuck in stress metabolism or low redox.
Fix:
- Consume a cleaner carb source - some carbs can give you brain fog
- Go low FODMAP
- Combine with more lean protein
- Add niacinamide + aspirin daily (lower stress metabolism).
- Ensure DHEA-S, testosterone, and thyroid are supported.
- Focus on warmth and relaxation, oxidation increases dopamine sensitivity.
- Address sleep and gut first if libido is still flat after 2 weeks.
9. Plateau After 2–3 Weeks
Likely cause:
Mitochondria adapted; need deeper support.
Fix:
- Add PQQ (10–20 mg) + CoQ10 (100–200 mg) + succinate (500 mg).
- Lightly reintroduce exercise intensity to increase mitochondrial demand.
- Cycle methylene blue (1–2 mg/kg) for a week to boost ETC throughput.
10. Everything Looks Good Except Glucose Still High in Morning
Likely cause:
The Dawn Effect — cortisol + GH rise before waking, raising FFAs and glucose.
Fix:
- Lower cortisol
- Lower endotoxin
- 1 g aspirin + Pyrucet on waking = eliminates FAO-induced insulin resistance.
- Wait 30 minutes, then have a carb-rich breakfast.
- Or keep breakfast lower-carb + protein until cortisol drops, then add starch/carbs later in the day.
Morning glucose normalizes fast once FAO is suppressed.
Summary: Troubleshooting in One Line
- High glucose → lower fat, add PDH support
- Crashes → improve oxidation
- Cold → increase carbs/thyroid
- Wired → calm redox
- Bloat → fix gut, not carbs
- Bad sleep → stabilize glycogen
The 14-Day Oxidation Reset
This is the implementation phase, two weeks to retrain your metabolism to oxidize carbs cleanly again.
You’ll be tracking warmth, energy, glucose curves, and sleep.
By Day 14, you should feel calmer, stronger, and noticeably warmer, with steadier glucose and deeper recovery.
Days 1–3: Baseline & Reset
Goal: lower fatty-acid oxidation and set your glucose baseline.
- Lower dietary fat to <40 g/day, cut all PUFA.
- Keep carbs moderate (150–200 g/day) from fruit, juice, potatoes, rice and honey.
- Record fasting glucose, post-meal curve (15/30/60/90/120 min), pulse, and temperature.
- Add:
- B1 (300 mg) + Mg (200 mg) daily.
- Niacinamide (250 mg 2×/day).
- Aspirin (325 mg morning).
- Goal metrics: fasting < 90 mg/dL, warmth increasing, energy stabilizing.
Days 4–7: Unlock Oxidation
Goal: re-activate PDH and suppress fatty-acid oxidation.
- Increase carbs to 250–300 g/day; keep fats low.
- Add Pyrucet (≈6 mg/kg/day) split around carb meals.
- Optional Meldonium (250 mg 2×/day) if you were long-term low-carb.
- Raise B1 → 600 mg, Mg → 400 mg.
- Continue Niacinamide + Aspirin stack.
- Expect: better sleep, warmer hands/feet, calmer mind, glucose peak < 130 mg/dL.
Note:
If mornings still show high glucose, add 1 g aspirin + Pyrucet on waking to flatten the dawn effect.
Days 8–10: Drive Redox & Mitochondria
Goal: build redox power and improve electron flow.
- Carbs → 350–400 g/day.
- Add:
- PQQ (20 mg) for mitochondrial biogenesis.
- CoQ10 (100-200 mg) + Vitamin K2 (5 mg) + Vitamin C (1 g).
- Optional Methylene Blue (1 mg/kg) if tolerated.
- Train 3–4×/week with moderate resistance sessions (avoid fasted training).
- Expect smoother energy, better focus, and post-meal temps near 37 °C.
Days 11–14: Full Oxidation Mode
Goal: high-flux glucose metabolism and stable hormones.
- Carbs → 450–700 g/day depending on tolerance.
- Keep fats < 40 g.
- Maintain Pyrucet + Aspirin combo.
- Continue B1, Mg, Niacinamide, and ETC stack (PQQ, K2, CoQ10).
- Optional DCA (12.5 mg/kg) every 3rd day for PDH surge (only with B1 support).
- Monitor:
- Fasting glucose 70–80 mg/dL
- 2-hour post-meal near baseline
- Steady warmth and calm energy
- Deeper sleep, morning wood, improved drive
By now, you’ll feel it: food fuels you instead of sedating you.
You’re burning carbs, not fighting them.
Maintenance After Day 14
- Keep your oxidation stack (Pyrucet + B1 + Mg + Niacinamide) daily.
- Cycle aspirin (5 days on / 2 off).
- Keep carb intake high relative to fat to maintain PDH dominance.
- Continue tracking temps, pulse, and glucose once a week to catch early drift back into FAO.
Expected Results
Within two weeks you should notice:
- Warmer baseline body temperature
- More stable glucose and energy
- Deeper sleep and calmer mood
- Higher libido, motivation, and recovery speed
- Noticeable muscle fullness and vascularity
This is the metabolic sweet spot — where glucose isn’t “spiking” but fueling high-performance physiology.
Conclusion — Keep It Simple
In most cases, you don’t need supplements.
You just need to experiment with different carb sources — ones that don’t irritate your gut, cause inflammation, or trigger food sensitivities — and pair them with lean, high-quality protein. Track your blood sugar, your warmth, and how you feel.
That alone is often enough to restore proper glucose oxidation.
If your glucose spikes a bit during the first few days, don’t panic.
It’s normal. As your metabolism re-learns how to burn glucose, those numbers will drop naturally over the following weeks.
If, after about 2 weeks, things haven’t improved, that’s when you can start layering in targeted support:
- Glycine, taurine, and aspirin first — the simplest trio to lower stress metabolism and support oxidation.
- Then, if needed, Pyrucet, T3, and (B-complex) to push PDH and redox balance further.
- Only later, if your labs or symptoms justify it, bring in mitochondrial supports like PQQ, CoQ10, or methylene blue.
The goal isn’t to build a supplement empire.
Start with food.
Tweak.
Adapt.
And only then, add what’s missing.
Keep it simple.
Let your metabolism remember how to do the work it was designed for.
