Today, we're going to chat about blood tests. A lot of people truly believe that dry fasting destroys your health and that it will show up on blood tests. Today we are going to dispel those myths. These tests look at all kinds of stuff, from the complete picture of your blood, iron levels, cholesterol, how your thyroid is working, vitamin B12, and white blood cell counts. If you've done any of these tests, or are planning to, you should check out this article. It'll help you understand what each of them means and how they might change after you fast.
If you are like me, you love to see data when it comes to dry fasting. So this topic is going to be extra special for you. This blood test was taken after my 9-day dry fast. It was taken approximately 3 weeks after the fast, and it's a great snapshot of what it looks like. Take into consideration that I very recently had a severe autoimmune disease called long covid. Very recently I also went on a week-long spartan exercise regimen including heavy sauna use, weightlifting, and running. I had a small relapse (still very functional) which showed me that maybe everything has not yet been cleared.
This gave me an opportunity to try the Nicotine test, which is an interesting theory that evolved recently and has some really bold claims from people that have tried it. The theory focuses on the acetylcholine receptors and other possible cofactors. The idea is that nicotine has a 20x affinity to the receptors, which forces the covid spike protein and viral particles out of them. It's possible that the viral particles sit in those receptors and sort of hijack them, causing a lot of chronic fatigue syndrome symptoms. I've just completed the first week of the nicotine test and am now in the recovery week, and I've got to say, there were some potent experiences and I believe there's something there to explore. You can learn more about it in my blog post about the nicotine test on dryfastingclub.com.
So at this point, I've done multiple extended dry fasts and am believed to be fully (99%) recovered from severe long covid. The blood test shows that maybe things are still not 100% - even though the results are quite healthy. The reason I say this is because my iron levels could be slightly more optimal, and there are indications that there is still some possible inflammatory anemia occurring. This means that there is still an underlying condition that is slightly triggering iron absorption. In these cases, the best course of action is healing the underlying condition, and in this case, it would be the lingering long covid particles. But let's focus on the most important blood markers when you're talking about dry fasting. GFR - the glomerular filtration rate (the pronunciation of glomerular is tough!), creatinine levels, Alanine aminotransferase, sodium, and potassium levels. We'll also talk a bit about TSH - thyroid stimulating hormone, and mention some tests that could have given us a bit of a better look. T3 and T4 tests.
We're not going to talk about my amazing a1c marker level which indicates blood glucose history and is the best diabetic blood marker, and we can skip the perfect red blood cell and white blood cell levels.
Blood tests can indicate if you're struggling with certain vitamin and mineral deficiencies, certain immune problems, kidney filtration, blood sugar levels including A1C markers, and hormonal levels. Someone with lowered kidney filtration needs to approach dry fasting entirely differently from someone with mineral deficiencies. At the same time, kidney filtration issues can affect mineral deficiencies. It's a big circle with everything intertwined.
It's always a bit of a puzzle and that's where experience and the ability to decipher symptoms and blood markers becomes critical. In this post, I'll take you through one of my most recent blood tests which was performed approximately 24 days after completing a 200-hour hard dry fast. The refeed was very strict for the first 9 days, followed by a much more lenient dietary regimen. For this refeed I followed the Filinov protocol and documented the whole thing, you can see that under the Filinov refeed protocol guide article. Keep in mind that I do not refeed like this normally. The dietary regimen that I do is explained in the current scorch protocol "in-between" fast snapshot. You can find the scorch protocol here.
I will do my best to target overarching and key information for each test so that you can make the necessary connections yourself when you get your own test done.
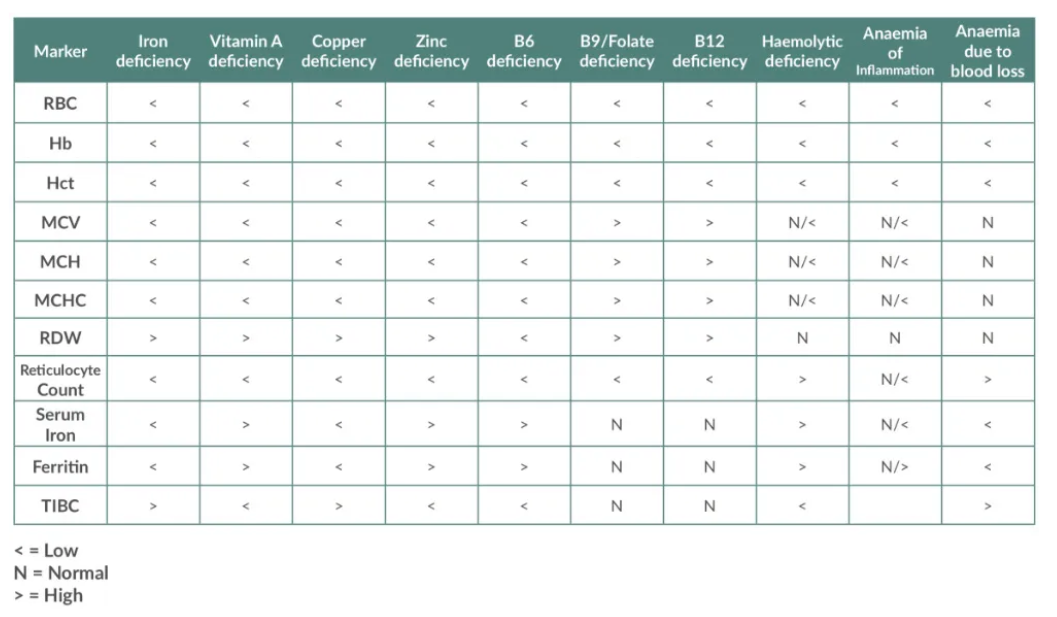
This is a table that can be used to quickly scan and analyze deficiencies at a surface level:
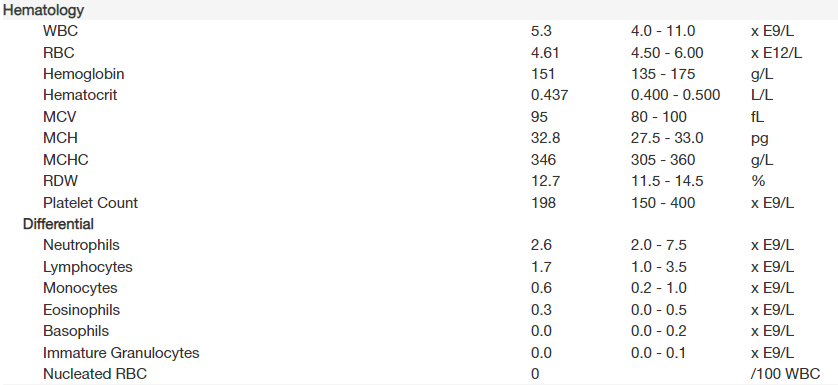
Full blood test results here
We'll be breaking them down so that you can better understand your own, and get a deeper insight into my tests and experience with dry fasting results.
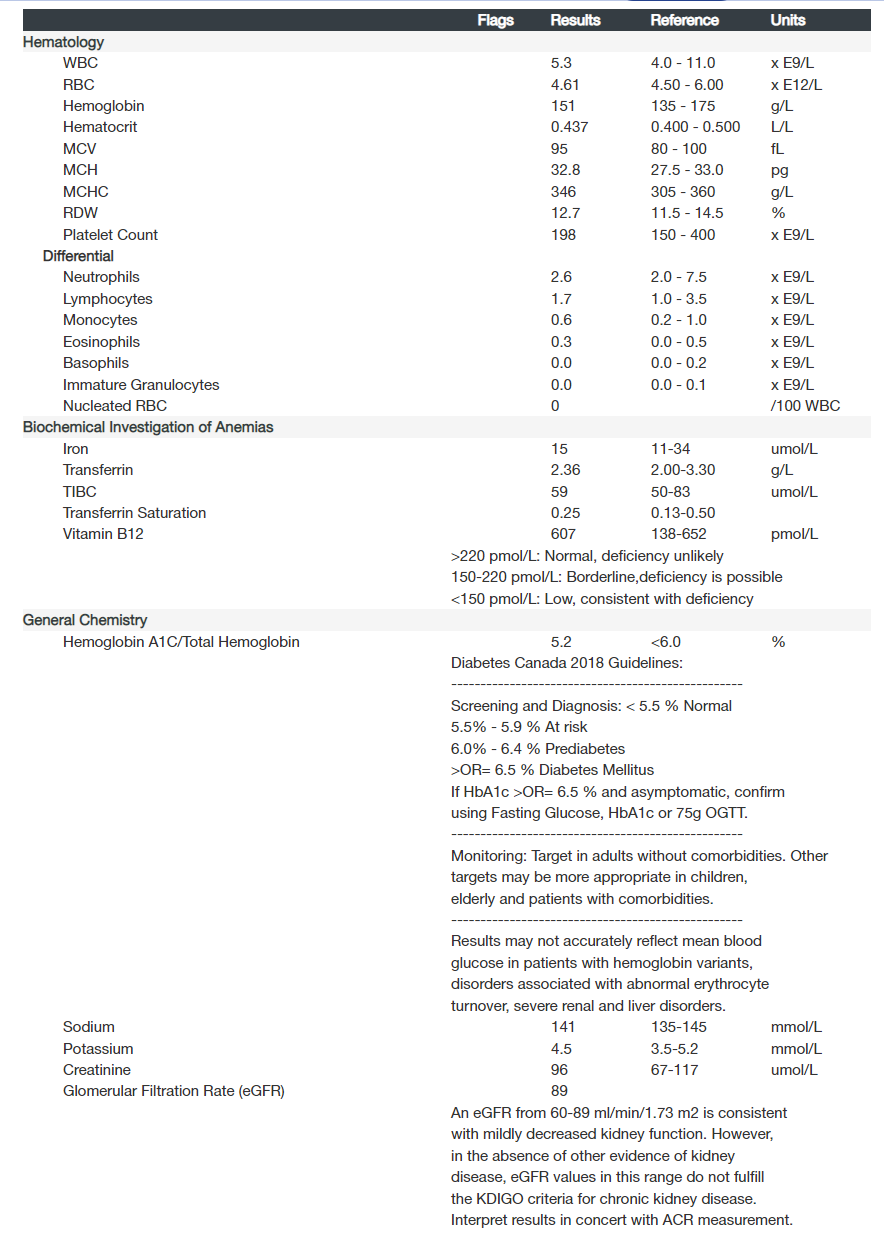
Can you believe some of these numbers? Considering I was bedridden, had derealization, MCAS, Gut problems, memory problems, trouble breathing, chronic fatigue, and nonstop migraines, I believe I have bounced back quite healthily. I know I most likely had organ damage, filtration issues, liver issues, and blood clots. A lot of people think that a 9-day dry fast should kill you, and at the very least show severely affected blood markers. So let's dive into the numbers.
Hematology blood markers after 200HR dry fast
WBC
A high WBC count, known as leukocytosis, could indicate an infection, inflammation, an immune response, trauma, leukemia (blood cancer), or a response to certain medications. A low WBC count, known as leukopenia, could indicate bone marrow damage or failure, severe infections, certain autoimmune conditions, or a reaction to certain medications.
When it comes to high WBC counts it could mean numbers as high as 80(80,000) and even over 100 (100,000). This usually indicates leukemia or some sort of problem with the blood.
Neutrophils
Neutrophils are the most plentiful type of white blood cell and serve as defenders against infections. They play a key role in your body's inflammatory response, aiding in the removal of damaged cells and invading microorganisms. Lower neutrophil levels could imply a weakened immune system, whereas elevated levels could indicate a bacterial infection or increased inflammation.
Neutrophils = 40–60%. Higher = viruses, autoimmunity, or detoxification challenges
Lymphocytes
Lymphocytes serve as defenders in the body's fight against infections, accounting for approximately 25% of the total white blood cell count. Reduced lymphocyte levels can point to a compromised immune system, while elevated levels often signal infection (particularly viral) or an increased state of inflammation. Maintaining hydration and adhering to a well-balanced diet can enhance your immune system's performance.
Monocytes
Monocytes are cells that consume harmful bacteria and foreign particles in the blood. They typically constitute around 5–10% of the total white blood cell count. Elevated levels might signify an infection, whereas reduced levels could suggest increased vulnerability to infections. While you can't directly impact your monocyte count, proper nutrition can enhance the overall efficiency of your immune system.
Monocytes = 0–7%. Higher = liver dysfunction, prostate problems, or recovering from infection (or Epstein Barr virus)
Eosinophils
Eosinophils are specialized cells that play a role in managing allergies and fighting certain infections. Elevated levels often indicate the presence of an allergy or a parasitic infection. They constitute only a minor portion (1–3%) of the total count of white blood cells. To boost your immune system's functionality, it's beneficial to stay well-hydrated and maintain a balanced diet rich in fruits and vegetables like tomatoes and carrots, along with herbs and spices such as turmeric and cumin.
Eosinophils = 0–3%. Higher = food sensitivities, environmental allergies, or parasites
Basophils
Basophils are part of the body's defense system against infections, comprising just 1% of the total white blood cell count. An unusually high basophil count could signal an infection or inflammation, potentially leading to fatigue and weakness. Given that they are the least common type of white blood cell, a low basophil count is typically normal. Even with low basophil levels, your immune system can function effectively. To boost your immune system's efficiency, ensure you get enough micronutrients like zinc, iron, and vitamins A, C, and E, and stay well-hydrated.
Basophils = 0–1%. Higher = tissue inflammation
Nucleated RBC
Nucleated red blood cells (nRBCs) are immature red blood cells that still contain a nucleus, which is typically lost as the cells fully mature. They are normally found in the bone marrow, where red blood cells are produced, but not in circulating blood. The presence of nRBCs in a blood sample is unusual and typically suggests that the body is producing red blood cells at an increased rate, possibly due to severe anemia, significant blood loss, or certain illnesses like cancer. There's no specific level that indicates a problem, as nRBCs aren't usually present in the blood at all.
WBC Tests Conclusion
Remember some key things here. Vegans who have been on the vegan diet for quite some time can show much lower WBC and sometimes in the area of 3-4. This is usually considered fine, and doctors don't worry until the number drops to 2 and below. You can expect a lower WBC count directly after a dry fast, so it's good to wait a few weeks before testing after a dry fast. If you're able to check multiple times, then it's fun to watch your numbers, and you can take a test during, right after, and a few weeks after a dry fast.
A WBC test usually indicates if your body is actively fighting an infection, or if you have markers of severe diseases like cancer. It's not a crucial marker for after a dry fast unless you have data from before you dry fasted. Then you can use it to see the difference. If you were healthy before the dry fast, you can expect similar numbers afterward. If you take the test too early, you will notice that your WBC numbers are low, since the immune system rebuilds a large portion of itself post-fast. Remember that neutrophil levels can fluctuate depending on the time of day.
My count was 5.3 or 5,300. This is in a very healthy low inflammation range. It's near the lower end of the range, but it's important to remember that the healthier you are the lower you should be on this range (without dipping too low). Some people panic if their WBC count is near 4, and if you want to aim right for the middle you'd want to be around a 7-8. However, some researchers agree that if we use healthy inflammation levels (based on a c-reactive protein test) to set "normal" white blood cell count, the "healthy" range would be 3.11 - 8.83. If we take this into consideration, anything around a 5 to a 6 would be the optimal range. Score! Anyways, it just goes to show how subjective a lot of health tests can be, and that the truth is often hidden in between the lines.
RBC
For men: 4.5 to 5.5 million cells per microliter of blood
For women: 4.0 to 5.0 million cells per microliter of blood
A high RBC count, known as polycythemia, can occur due to conditions that cause low oxygen levels in the body, such as lung diseases or heart problems. It can also be seen in a disorder called polycythemia vera, where the body produces too many RBCs. Too many RBCs can mean thicker blood and clotting issues. Some people need therapeutic phlebotomy to manage symptoms. A low RBC count, or anemia, can be caused by several conditions including nutritional deficiencies (such as iron, vitamin B12, or folate deficiency), blood loss, bone marrow disorders, chronic kidney disease, or certain inherited conditions like sickle cell anemia or thalassemia.
Always remember that if you fall into a healthy range, you should feel very good, it's usually only when you fall out of the range, you should take a closer look. Sometimes even numbers slightly out of the range are not a cause for panic.
Hemoglobin (Hb):
Hemoglobin is the protein molecule in red blood cells that carries oxygen from the lungs to the body's tissues and returns carbon dioxide from the tissues back to the lungs. Hemoglobin levels are expressed in grams per deciliter (g/dL) of blood. The normal range for hemoglobin is typically around 13.5 to 17.5 g/dL for men and 12.0 to 15.5 g/dL for women. Lower than normal levels can indicate anemia, while higher levels might indicate polycythemia (an excess of red blood cells).
How to raise hemoglobin?
Addressing deficiencies of iron, b12, and folate is a good place to start. Testosterone and EPO injections are banned in sports, but they work as well. Testosterone actually stimulates EPO production. Some athletes train at altitude, but the benefits usually return to baseline pretty quickly. The best way is to exercise regularly, and eat well. Fasting helps you regulate your hemoglobin and bring it into optimal ranges for health. However, fasting does not give you optimal athletic hemoglobin levels. For that, you need to build an exercise routine post-fasting. I use a strategic approach to all of this for the scorch protocol for healing long covid and not only bring you back to baseline health but to an even better place.
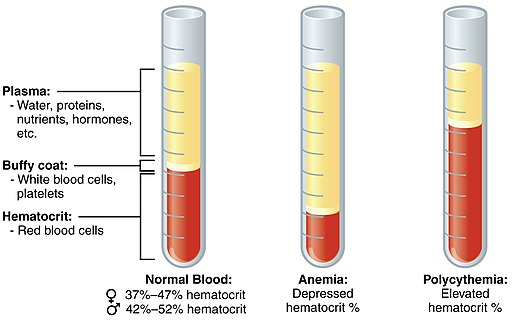
Hematocrit (Hct):
This measures the proportion of your blood that is made up of red blood cells. It's usually expressed as a percentage. For instance, a hematocrit of 45% means that 45% of the blood's volume is composed of RBCs. Normal ranges are approximately 38.8% to 50.0% for men and 34.9% to 44.5% for women. Low hematocrit can be a sign of anemia, blood loss, or bone marrow problems, while high hematocrit can suggest dehydration or polycythemia. Lower levels might imply anemia, a condition where your tissues don't receive enough oxygen, leading to fatigue. Iron is crucial for red blood cell production. While red meat is a prime source of iron, individuals adhering to a vegetarian or vegan diet might face challenges in obtaining sufficient iron.
RBC indices
These indices can help to identify the cause of anemia. MCV, MCH, and MCHC.
Mean Corpuscular Volume (MCV):
This measures the average size or volume of a single red blood cell. It's used to help diagnose the cause of anemia. MCV is measured in femtoliters (fL) and the normal range is about 80 to 96 fL. If the MCV is lower than normal, it suggests that the red blood cells are smaller than normal (microcytic), which can be seen in iron deficiency anemia or thalassemias. If the MCV is higher than normal, the red blood cells are larger than normal (macrocytic), as seen in vitamin B12 or folate deficiency.
Mean Corpuscular Hemoglobin (MCH)
This measures the average amount of hemoglobin in a single red blood cell. It is calculated by dividing the total hemoglobin amount by the number of red blood cells. Normal values are around 27 to 31 picograms/cell. Abnormalities can suggest various types of anemia and are often considered with MCV values.
Mean Corpuscular Hemoglobin Concentration (MCHC)
This measures the average concentration of hemoglobin in a given volume of red cells. It's basically a calculation of the amount of hemoglobin relative to the size of the cell. Normal values are usually around 33.4 to 35.5 g/dL. If the MCHC is low, the cells are hypochromic or lighter than normal, which can occur in iron deficiency anemia. If the MCHC is high, the cells are hyperchromic or darker than normal, though this is rare and can be seen in hereditary spherocytosis (a condition that affects red blood cell shape and function).
High normal levels of MCHC indicate that the hemoglobin concentrations are really good and your blood cells are working efficiently.
RDW (Red Cell Distribution Width)
This is a measure of the variation in size of your red blood cells. In other words, it tells you how similar or different (in size) your red blood cells are. A normal RDW is typically between 11.0 and 14.5 percent, but this range can vary slightly between labs. If your RDW is higher than normal, it means your red blood cells are more varied in size than usual, which is often seen in conditions such as iron deficiency anemia and vitamin B12 deficiency.
Platelet Count
Platelets, also known as thrombocytes, are tiny blood cells that help your body form clots to stop bleeding. If one of your blood vessels gets damaged, it sends out signals that are picked up by platelets. The platelets then rush to the site of damage and form a plug, or clot, to repair the damage. The normal range for a platelet count is usually between 150,000 to 450,000 platelets per microliter of blood, but this can vary slightly between labs. A low platelet count (thrombocytopenia) can increase the risk of excessive bleeding, while a high count (thrombocytosis) could potentially lead to abnormal clotting.
RBC Conclusions
Personally, I would prefer to have my RBC count in the 5 range, specifically for better cardiovascular endurance. But considering the body is still rebuilding after the fast, and I feel great, then I have nothing to complain about. Also, when it comes to lower range normal, it can indicate good health because it shows that the body is not being stressed into overproduction of RBCs. Low oxygen levels are some of the most popular situations that cause an increase in RBCs as your body tries to adapt to a low-oxygen environment by producing more RBCs so that they can deliver more oxygen to the body. Think of the stories of soccer players training in the mountains to increase their RBC count naturally. Many doping drugs in sports cause an increase in RBCs to improve oxygenation. A popular one is EPO injections (erythropoietin) which is a substance created by the kidneys that signal to the bone marrow to create more RBCs.
Raise EPO levels naturally by Using the Sauna, Eating Beets, Massaging your Kidneys, and Taking echinacea supplements.
However, it's important to keep in mind that a low RBC count can indicate kidney disease and is something to keep an eye out for with dry fasting specifically. From most of the anecdotal evidence, we can confirm that if you are doing a well-paced, well-regulated dry fast, you can actually improve your kidneys. But, if you're being reckless and overdoing it then you need to keep an eye out on your kidneys, and being aware of the blood levels is critical. Seeing chronically low RBC counts, as well as lower GFR Glomular filtration rates, need to be addressed.
Iron - Biochemical Investigation of Anemia
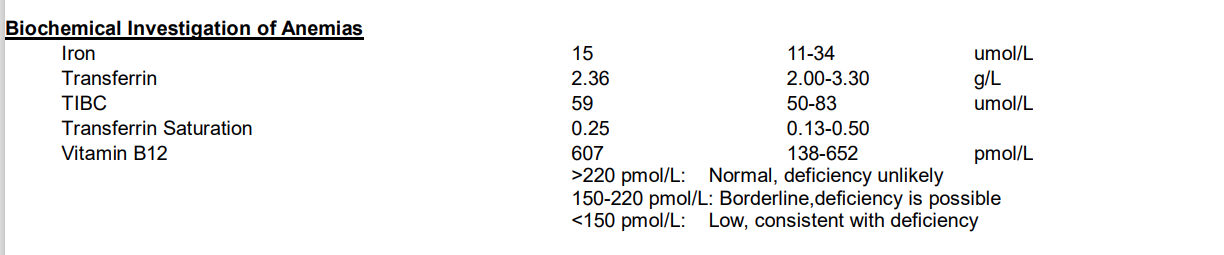
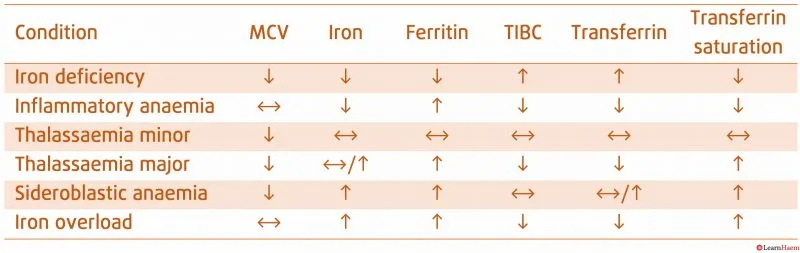
We'll talk about each blood marker for Anemia. But I want to dial in a little bit on the one I think relates to most of us here looking to heal autoimmune diseases (long covid included). I had much worse anemia markers earlier in my long covid adventure. When I advise people who are suffering from an autoimmune disease and iron/TIBC/transferrin issues, even though they are heavily supplementing with iron, I always say that I believe the problem lies with Inflammatory anemia which is also known as "chronic disease anemia".
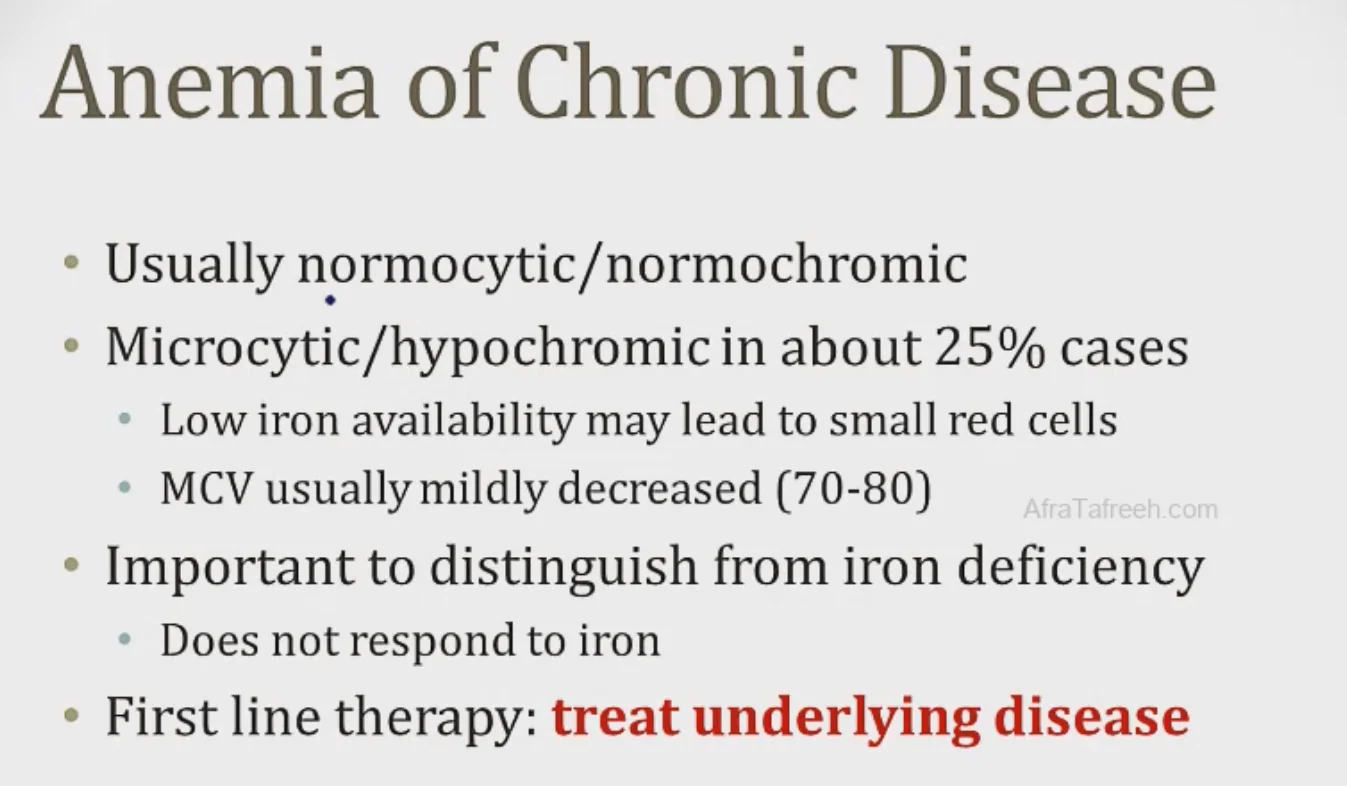
Important - The key here is that iron supplementation does not work until the underlying disease is targeted. Think of it as the body hiding the iron that is already there. The evolutionary goal of hiding iron during inflammation is to hide the iron from bacteria, which need iron to grow. The additional iron will continue to be sequestered and not even absorbed as much in the intestines. Meaning that your iron levels won't go up. We'll leave it at that for now.
My doctor said to just come back after a couple months and take it again.
This is the problem with centralized medicine. Getting into the nitty gritty requires someone to focus solely on you and what makes you tick. Your history, symptoms, and lifestyle. Without it, you are just another number, and it's much easier to separate a group of 100 into 3 boxes, instead of the 100 they deserve.
If you believe you're suffering from inflammatory anemia, the only real cure is to treat the underlying disease. In this case, it's usually a persistent virus, damaged immune system, and/or damaged metabolic pathways. That's why so many people find relief through fasting. It targets and resets both metabolic pathways and your immune system, while simultaneously dehydrating and ripping apart pathogens in your body.
Ferritin
iron stores in macrophages and liver (this is storage form: a protein that also made in the liver to hold on to ferritin, you can't have it on the highway i.e. in the blood). People often use the safe analogy for ferritin, when you have chronic disease or infection (you try to keep iron away from the bugs), you lock your iron away in the ferritin safe.
Iron
A measure of iron in the blood (raw amount)
Transferrin
Transporter of Iron.
TIBC
TIBC (total iron-binding capacity): a measure of transferrin molecules in the blood. Note: transferrin is a protein made by your liver specifically for this purpose (think of it as a car/truck/carrier for your iron)
Transferrin Saturation
Transferrin saturation, calculated from iron and TIBC (Total Iron Binding Capacity) results, provides insights into the body's iron status. Low transferrin saturation typically suggests iron deficiency, while high levels indicate an excess of iron. Both extremes can lead to a host of adverse health effects, including fatigue, headaches, and weakness.
The percentage of transferrin molecules that are bound by iron is ~ 33% roughly at all times (so on the highways, only 33% of the cars have passengers). Percentage Saturation can also be viewed as how much of the total transferrin floating around is actually bound to iron. Normal is usually around 33%.
Understand what each values represent and mean and you can work out the rest. In iron deficiency, for example, iron stores fall (you are deficient), so ferritin is low. Compensation is to increase TIBC (by increased TF). % Saturation; which was how much Iron is actually bound to TF would reduce, because you now have more TF in the setting of relatively unchanged iron.
Iron/Anemia Conclusion
When you're dealing with possible iron deficiencies while sick with an unknown illness or autoimmune condition, you are most likely running into a scenario where your iron levels, transferrin, TIBC, and Transferrin Saturation are low. Often your ferritin may be high as well. This all indicates inflammatory anemia. You can go absolutely crazy trying to piece together all the different possibilities, and you'll see thousands upon thousands of threads online with people trying to figure out how to deal with their iron levels. I'm not here to discuss the hundreds of different theories on how to improve your iron levels. I don't believe in iron supplements if you're eating a good diet. As with most vitamin and mineral levels, it all starts with your digestion. Think stomach acid, villi length, and leaky gut.
When you have inflammatory anemia, your iron absorption is limited as well. The only foolproof solution to this problem is to deal with the underlying condition. This could be healing from the disease causing the inflammation (in my case, it would be long covid). If anyone thinks they have the perfect supplement for you, then you need to be aware that it most likely won't work because of the Swiss cheese explanation. Your body is not full of holes, doctors are going to try to plug one or two of them, but they're not aware that you can't just focus on one thing. This is where fasting comes into play. Chaperone-mediated autophagy does not discriminate. If you give it enough time, your body will be able to throw the diseased and damaged cells, and pathogens into lysosomes for acidic dissolution! With that, you'll be able to heal gut absorption issues AND deal with the disease condition causing the inflammation. Focus on rebuilding the foundation so that everything else starts to work on the surface level.
Vitamin B12
The body obtains Vitamin B12 from dietary sources, and its levels are commonly assessed in conjunction with folate. Just as folate, Vitamin B12 significantly contributes to the formation of healthy red blood cells and additionally supports nerve health. Maintaining both vitamin B12 and folate within their respective normal ranges is crucial to prevent various types of anaemia and sustain regular energy levels. A deficiency in B12 can result in anaemia.
Since I'm focusing on my test I would say that I am sporting a pretty high b12, even though it's in the normal range. Normally people that panic are the ones that are hitting 900+ for their b12 levels. However, compared with a few other possible markers, I would consider inflammatory anemia, some people call this "autoimmune pernicious anemia". Or at least a risk for it. Inflammation can cause a false high b12. In this scenario, it makes perfect sense if you consider that there is still more long covid damage to heal, even though that would be a little depressing for anyone just starting on the long covid healing journey. However, keep in mind that I am back to living my life like before, I am also running, but I do feel a little rough if I overdo it (5K and up), so I'm aware there's still a few percent to go. I am also doing a liver flush, so I hope to get 2-3 done before my next blood test.
Hemoglobin A1C - Diabetes Risk
I've seen data on 153 healthy non-diabetics that wore CGMs (continual glucose monitors) - those are monitors that are constantly injected into your blood and monitor your glucose levels in real time. So you can eat something and watch exactly how your blood glucose levels react to it. Sinclair, a longevity expert I follow from time to time, talks a lot about his CGM and how he found out that grapes and white rice spike his glucose, but potatoes surprisingly, do not. Back to the topic, the 153 healthy non-diabetics, their average A1c was 5.1%
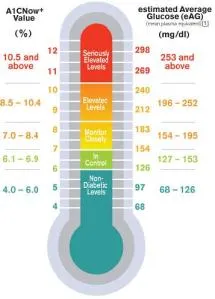
Aiming for an A1c of 4.5 to 4.6 is basically impossible even for someone not insulin resistant. That’s an average glucose of 82. Unless you’re gonna go zero carb carnivore I don’t see how it’s possible, much less sustainable.
The problem is defining healthy, it's getting rarer nowadays. The Dutch took a cross-section of about 3,000 non-diabetics, of all ages & all weights. Turned out the average A1c was 38(5.6%).
When 1/3 of the population is diabetic or pre-diabetic the bell curve has been pulled well to the right.
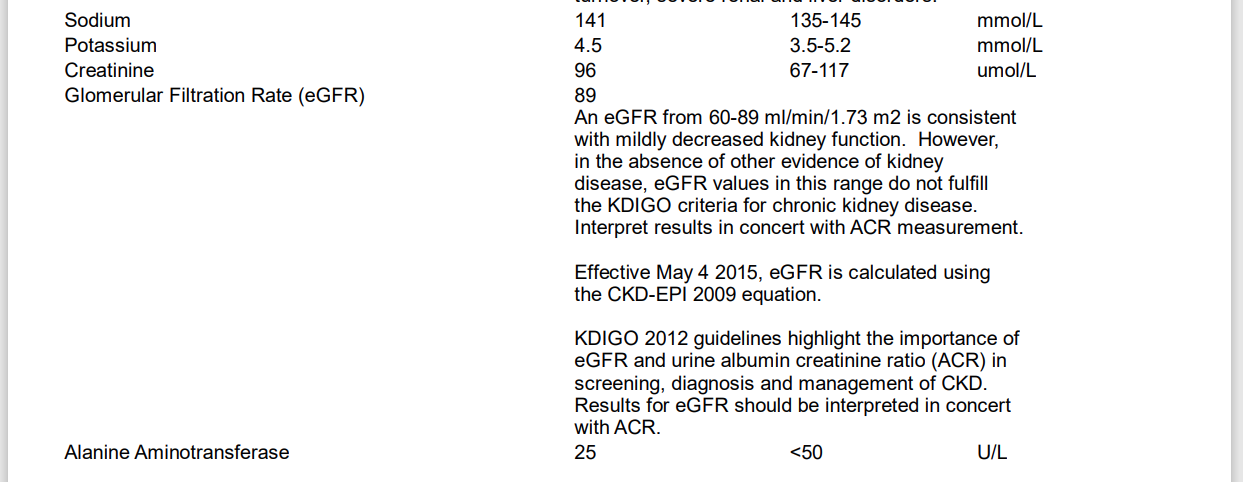
Sodium, Potassium, and Creatinine
Sodium, Potassium, Magnesium, Calcium, and Phosphorus
The 5 pillars of electrolytes and minerals in the body. I'm not going to go into detail about the importance of other minerals, even though we'll talk about Iodine a bit more later. But let's get to it. Is it possible to have a mineral deficiency with normal blood levels of said mineral?
The answer is Yes. Many elements of blood chemistry have tightly regulated homeostasis in the blood, and buffer or deposit in larger reservoirs that are invisible to blood tests.
Magnesium is a good example. Serum Mg tests are not that helpful because even a person with chronically low intake will generally have normal blood Mg levels, because it’s being pulled out of bones to buffer the blood concentration.
There are 5 main mineral tests:
Serum, RBC, Ionic, EXA, and Test Loading/Tolerance Test
The serum test measures levels in your blood serum. Most doctors order this test if they suspect a deficiency. The drawback with the serum test is that the majority of minerals in our bodies reside in our cells: serum contains less than 1% of our total minerals. So it is quite possible for the mineral levels elsewhere in your body to be low but have the serum test come back normal.
The RBC test is slightly more accurate. The RBC test is a blood test much like the serum test. The difference is that it measures the amount of minerals in the red blood cells. The RBC test is considered more accurate than the serum test because when you are low in a mineral your body takes it from cells for use elsewhere.
The Ionic test is just as accurate as the RBC test and looks at magnesium ions.
The EXA Test determines mineral levels from a tissue sample that is scraped from inside the mouth and then tested. This is done for a few minerals like magnesium. It's a hard test to find but is more accurate than the previous 3. The problem here lies in the fact that it only takes a snapshot of cells inside your mouth.
The Tolerance Test is the gold standard for mineral deficiency. It involves being injected with the mineral. For example magnesium. You then need to provide a few different urine samples as the body utilized the magnesium. The idea is that if most of it is absorbed, it shows that you are deficient, and if most are excreted, you know the body has good enough levels.
Conclusion
I am a big fan of supplementing magnesium and potassium. Eating a good whole foods diet usually makes sure you get a good amount of essential minerals. There's a correlation between eating more potassium and magnesium foods to increase longevity, while eating more sodium regularly, actually decreases longevity. This has to do with the overconsumption of sodium in our diets. Salt is added to everything as a flavor improvement, and to help preserve the food. Foods high in salt are designed to appeal to our taste buds and can often lead us to crave more. This is why the Standard American diet is so high in sugar and salt, while low in everything else. Profits over health.
There's a big reason all my protocols involve potassium and magnesium. Bone broth and eggs provide a very bioavailable source of phosphorus and all other minerals. I'm also a fan of green juices that are low-carb, and if strapped for time, greens powders from trusted sources.
Creatinine
Creatinine is a chemical waste product generated from muscle metabolism. It is produced from creatine, a molecule of major importance for energy production in muscles. Routinely, it's filtered from the blood by the kidneys and expelled in the urine.
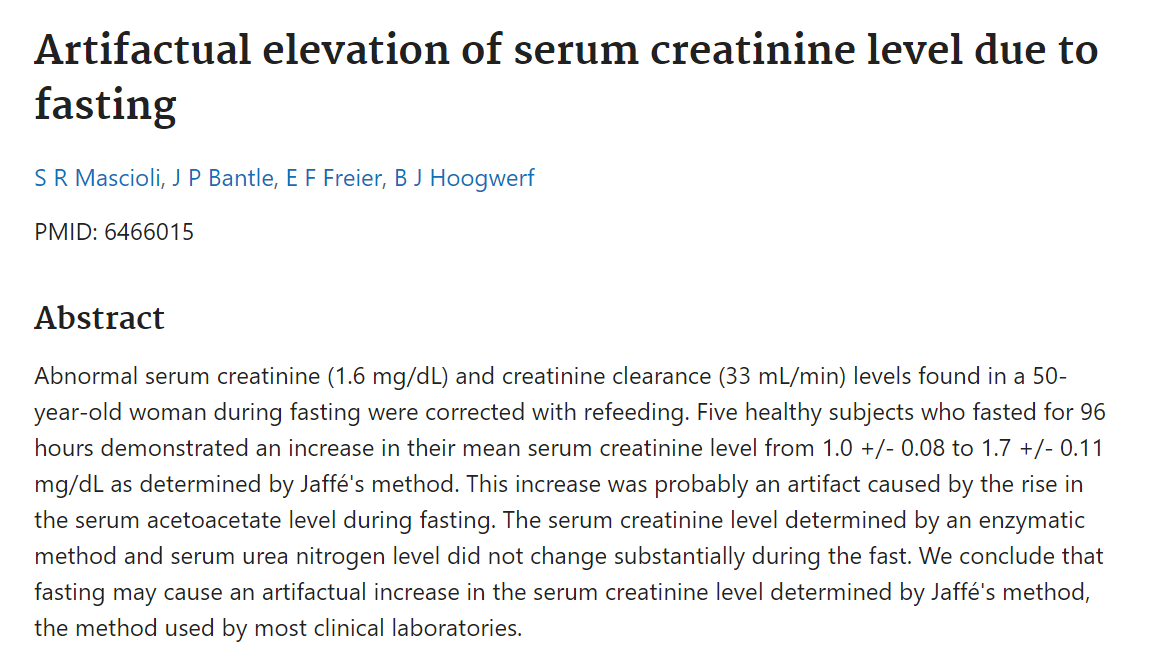
The assertion is that creatinine is overestimated in the common clinical lab method due to the increased acetoacetate levels from prolonged fasting. eGFR uses the incorrect creatinine value and ends up being overestimated. They note that creatinine levels tested through an alternate method showed no increase.
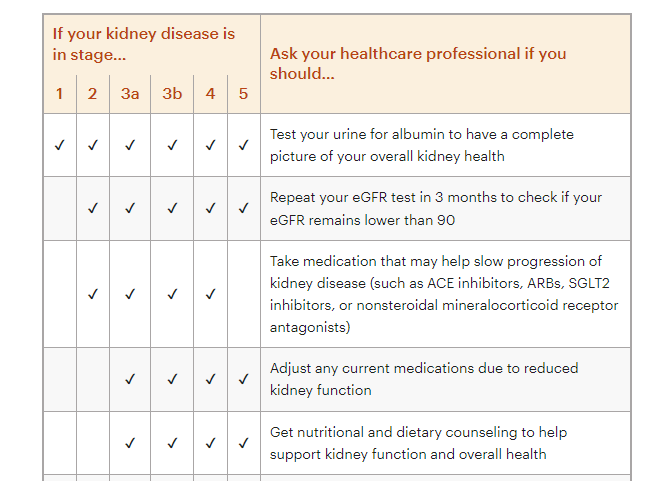
eGFR - Estimated Glomerular Filtration Rate
eGFR is used as an indication of how well your kidneys are functioning. Testing GFR directly is complicated, levels are therefore estimated based on your creatinine levels. Results can be influenced by a number of factors including muscle mass and weight. Individuals with high muscle mass will have higher levels which may be outside the normal range, and vise versa for individuals with low muscle mass. Creatinine and eGFR levels will rise immediately following strenuous exercise but should then return to baseline following recovery.
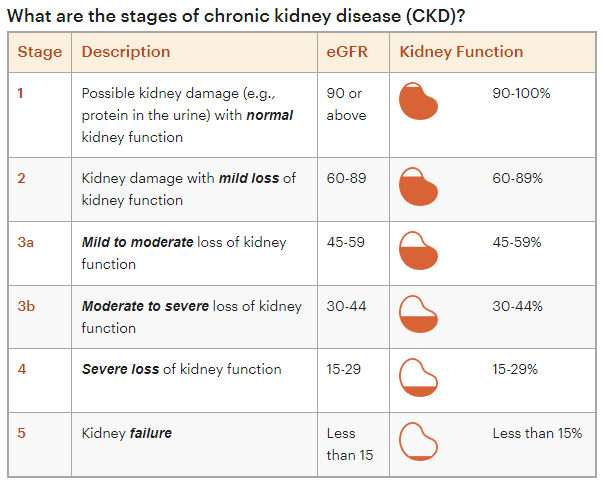
It's important to remember that eGFR, the glomerular filtration rate, is a calculation that takes into account your age, sex, and creatinine levels in the blood. Think of the kidneys as a filtration device that helps remove creatinine from the blood and into the urine. If it's not filtering correctly you can expect higher levels of creatinine in the blood. Side note: It also used to take race into account, but with political correctness, they've removed race-related calculations, to the detriment of scientific accuracy.
The race calculation showed that African Americans usually have a 2-5 ml/min/m^2 rate variation due to the "genetically larger muscle mass" hypothesis (on average). So all in all, this lends credibility to the fact that the more muscular you are, the higher your levels of creatinine will be shown. This can be misrepresented by a lowered eGFR score.
Right away this should give you an idea as to what to expect. High creatinine levels occur during extended fasting because of muscle catabolism buildup and can be expected in the first days of refeeding. Falsely high creatinine levels can also occur due to dehydration. Especially right after a fast, your body downregulates the metabolic water creation, and if you take a test during this time, it will look like you have terrible kidney filtration! Believe it or not, water fasts can have even higher creatinine levels than dry fasts because of electrolyte loss and higher muscle loss. You lose less muscle on a dry fast, and your body conserves electrolytes better, resulting in better hydration (as long as you are not overexerting yourself).
Creatinine can also run high the leaner you are as the body catabolizes more protein.
Important to remember that the eGFR is not a very accurate test when it comes to late-stage kidney disease where you need perfect accuracy. Sometimes cystatin is added with creatine for a better picture, but even then it could be off by a little bit.
How to help your GFR? There are many herbs and protocols out there that claim to help with kidney health. I really do not like diving into hundreds of herbs and supplements. My motto is KISS - keep it simple stupid, and the same goes for healing organ damage. If I am relatively healthy and want to heal my kidneys I would make sure I am eating a well-balanced diet, no processed foods, dry fast (and NOT water fast, because water fasting may actually damage the kidneys more than help due to electrolyte loss, higher muscle loss, and less metabolic deuterium depleted water creation), use adsorbents like activated charcoal at night or first thing in the morning, hydrate well in between dry fasts with clean water, hydrating fruits and vegetables (structured water) like watermelon, strawberries, celery, tomatoes, and cucumber, and good digestive and detox herbal teas like chamomile, peppermint, and specifically: dandelion root.
Conclusions
Taking into account that my number after 3 weeks of refeeding came back at 89, which is 1 point away from perfect kidney scores, means a lot. This is not my first rodeo. You need to be aware that I've done over 6 hyper extended dry fasts. (7 days and up) over the last 2 years, and a few shorter ones as well. Another thing to take into consideration is that I am very athletic, and love to lift weights and run. My body composition is on the above-average muscular side. Knowing this should make you understand that my eGFR score is already artificially suppressed, as most athletes and bodybuilders have better kidney filtration than the eGFR shows.
Alanine Aminotransferase
The enzyme called Alanine aminotransferase (ALT) is primarily present in the liver, with only minor quantities typically detected in the blood. However, any damage to the liver or muscles can result in a higher concentration of ALT circulating in the bloodstream. This elevation can be caused by excessive alcohol consumption or after intense physical activity. To maintain the health of your liver, it is advised to moderate your alcohol consumption according to suggested guidelines and incorporate nutritious foods into your diet, including whole grains, fruits, and vegetables.
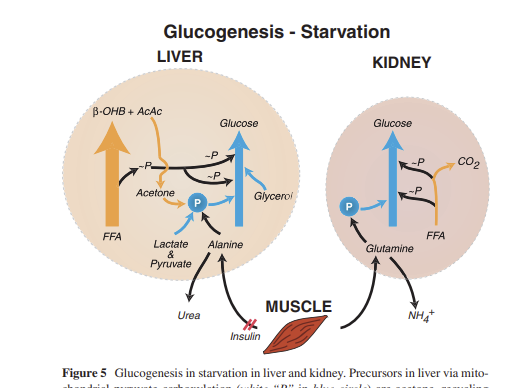
Alanine helps in gluconeogenesis and levels rise during extended fasting. Dry fasting for longer than 3 days will show a rise in alanine aminotransferase on blood tests. Muscle is broken down during gluconeogenesis to provide the required glucose. You can expect high ALT during a blood test or shortly after an extended fast. The levels should come back to normal range within 2-4 weeks of refeeding.
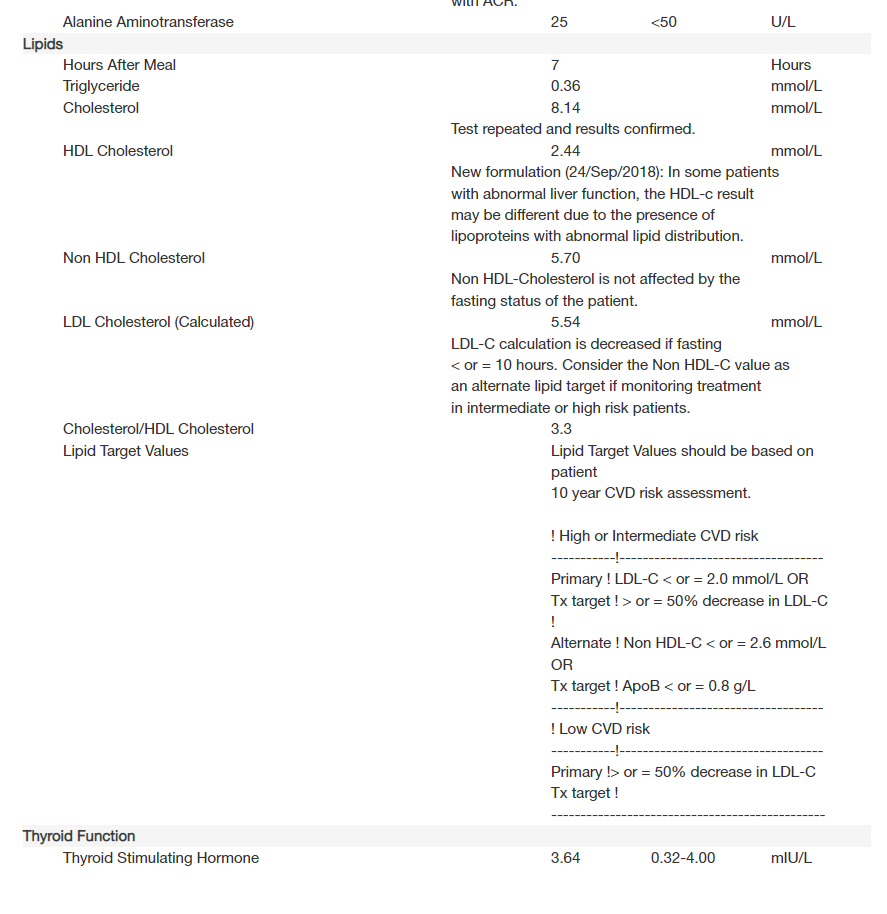
Lipids - Triglyceride, Cholesterol
A Lipid Profile is a tool used to assess the risk of heart disease and to guide treatment decisions if you're at borderline or high risk. This test, along with other identified heart disease risk factors, informs the creation of a treatment and follow-up plan. Depending on your test results and additional risk factors suggested treatments could range from modifications in diet and exercise to the prescription of lipid-reducing drugs, like statins. The Lipid Profile test includes measurements of Cholesterol, HDL (known as "good" cholesterol), LDL ("bad" cholesterol), VLDL, Triglycerides, and the ratio of "good" cholesterol to total cholesterol.
Triglyceride: 0.36 OR 31.8 mg/dL (multiplied by 88.57)
Total Cholesterol: 8.14 OR 314.7 mg/dL (multiplied by 32.87)
HDL Cholesterol: 2.44 OR 94.35mg/dL
Non-HDL Cholesterol: 5.70 OR 220.4mg/dL
Cholesterol has been demonized for a long time, although centralized medicine is finally coming around to the idea that elevated cholesterol levels are not always bad. In fact, our body creates cholesterol for a plethora of processes in the body. It is quite an important building block. If your health is improving, and you are fasting, high cholesterol levels may be a sign of a healthy body doing its thing.
Definitions of different lipid profiles
Total cholesterol. This is the sum of your blood's cholesterol content. It is just an overview of your cholesterol level. It might be misleading, as it combines good and bad cholesterol levels in your blood and does not give sufficient information about heart disease risks.
- Desirable: Less than 200 mg/dL
- Borderline high: 200-239 mg/dL
- High: 240 mg/dL and above
Low-density lipoprotein (LDL) cholesterol. This is called the "bad" cholesterol. Too much of it in your blood causes the buildup of fatty deposits (plaques) in your arteries (atherosclerosis), which reduces blood flow. These plaques sometimes rupture and can lead to a heart attack or stroke.
- Optimal: Less than 100 mg/dL
- Near optimal/above optimal: 100-129 mg/dL
- Borderline high: 130-159 mg/dL
- High: 160-189 mg/dL
- Very high: 190 mg/dL and above
High-density lipoprotein (HDL) cholesterol. This is called the "good" cholesterol because it helps carry away LDL cholesterol, thus keeping arteries open and your blood flowing more freely.
- Optimal: 60 mg/dL and above
- Borderline: 40-59 mg/dL
- Risk of heart disease: Less than 40 mg/dL
Triglycerides. Triglycerides are a type of fat in the blood. When you eat, your body converts calories it doesn't need into triglycerides, which are stored in fat cells. High triglyceride levels are associated with several factors, including being overweight, eating too many sweets or drinking too much alcohol, smoking, being sedentary, or having diabetes with elevated blood sugar levels. Triglyceride levels might be artificially high if you eat prior to your blood test.
- Normal: Less than 150 mg/dL
- Borderline high: 150-199 mg/dL
- High: 200-499 mg/dL
- Very high: 500 mg/dL or above
My Blood Cholesterol and Cholesterol Ratios
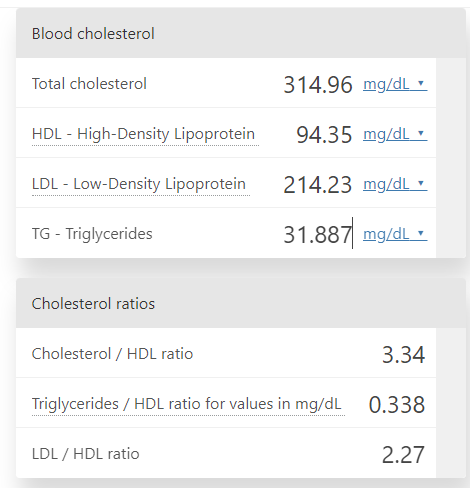
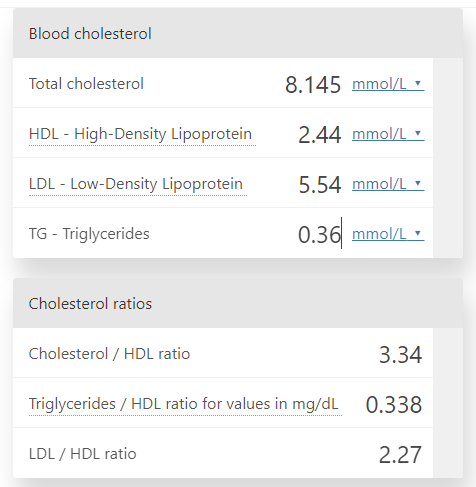
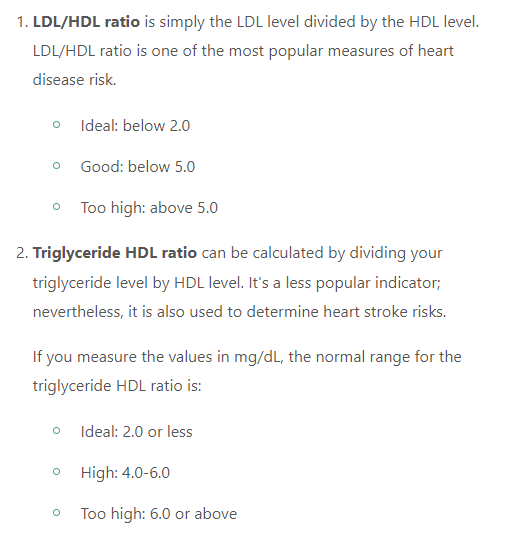
The Cholesterol ratios all fall into Ideal or near-ideal ratios. This is good. The ratios in this case are very similar to the Glucose-Ketone Index (GKI) which gives you a better picture of autophagy/ketosis levels than simply glucose and ketones separately.
You can see that the Triglyceride HDL Ratio is extremely low, and this is because my triglyceride levels are extremely low, while HDL is very high. Both are extremely desirable traits. The scariest thing that throws everything off is the LDL levels. It both increases my Total #s and LDL numbers.
If I were to follow standard total cholesterol levels, I'd believe that I was a walking heart attack waiting to happen. Ignoring the fact that my health has been consistently improving, my strength and endurance have been going up, and I literally jump out of bed with energy and go for a run each morning, I would truly be worried. But once you dive deeper, you start to realize that there is much more nuance to these readings, and this is something most doctors don't have time to get into. Once again. It's easier to place you in a box and move on.
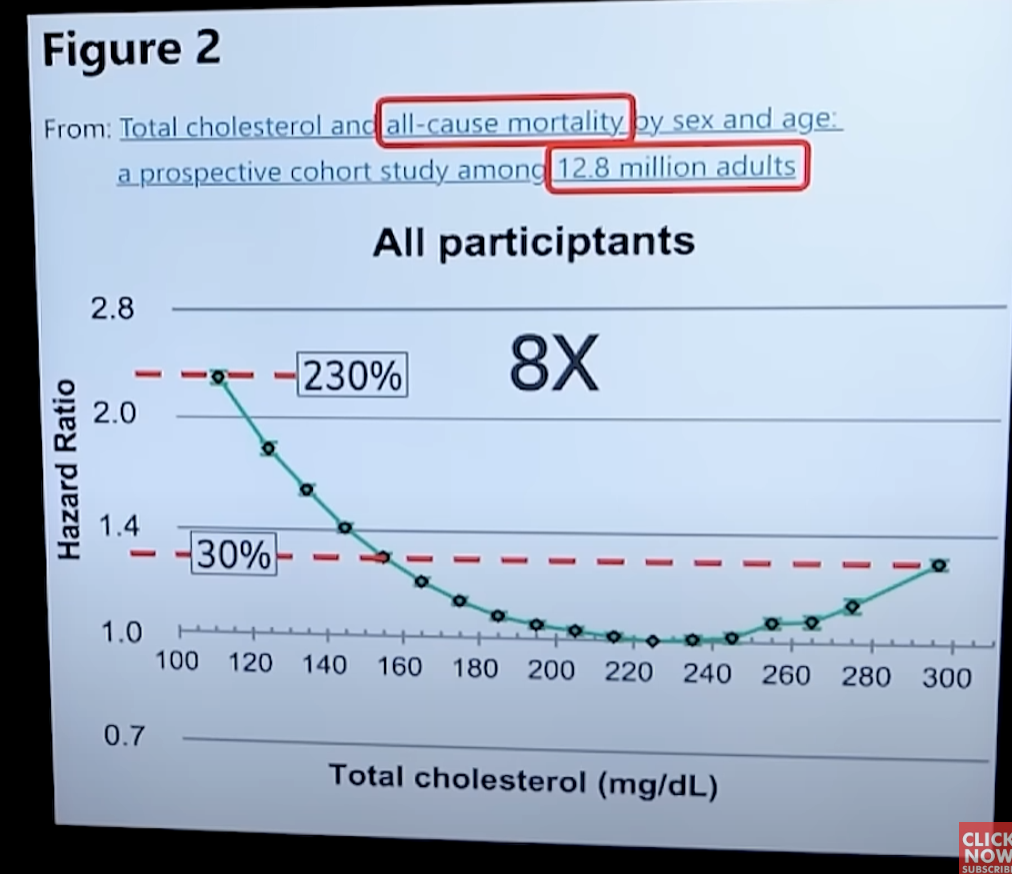
Before you panic when you see these kinds of cholesterol numbers even though you feel great, look at this study that looked at 12.8 million adults below. From the numbers you can see that even up to 300 mg/dL for cholesterol you are looking at only a 30% hazard ratio, while having very low numbers (under 160) you can get up to 230% more risk of dying. We have to take into consideration that a lot of unhealthy adults are also skewing these results, so logically, if you are overall healthy, and feel well with high Total Cholesterol, you may be perfectly fine. In fact, I'll always take slightly higher total cholesterol vs uncomfortably low cholesterol. Cholesterol is an important molecule for the human body.
Triglycerides
Managing triglycerides is crucial if you want to not have a heart attack or other forms of heart disease. This is because triglycerides occur in the bloodstream as something called VLDL particles that interact with LDL particles, causing them to become triglyceride-enriched, a process that causes small LDL particles to form. Recall that small LDL particles are a potent cause of heart disease. By keeping triglycerides at 60 mg/dl or less, you have minimized or eliminated small LDL particles and thereby heart disease risk. 60mg/dL is specified because at this number and lower, all small LDL particles stop forming (very good).
However, it's important to keep in mind that there may be some caveats. Low triglyceride levels are usually beneficial. If you are healthy and your levels are relatively low, you have nothing to worry about. Studies found low levels were associated with reduced risk of heart disease and death from all causes.
But! Abnormally low triglyceride levels have been linked with worse outcomes in certain conditions, such as heart failure. They have also been linked to autoimmunity. Low triglyceride levels are, in these cases, probably due to underlying issues such as inflammation or impaired liver function. Because I've battled long covid for so long, I have to keep in mind that potentially there is still lingering inflammation or my body is still building back since then. Since I deal with a lot of long covid and autoimmune patients, it's important to keep an eye on this and see how the levels change with subsequent tests. It's also important to consider how a liver flush can impact these numbers considering liver health may be a marker for low triglycerides. I will be performing 2-3 liver flushes over the next 2 months before I take another blood test.
Doctors consider any value below 150 mg/dL normal and under 90 mg/dL optimal. Low triglycerides can slightly overestimate LDL cholesterol. High HDL cholesterol and low triglycerides are usually beneficial and lower the risk of heart attacks.
Cholesterol Conclusions
Most people, even some doctors, still rely on these kinds of measurements, even though they're outdated and don't tell us much. It's time we stopped measuring things that don't really matter.
Some people, including a few doctors, understand this better. But even they don't have all the answers yet. There are parts of this puzzle we can't test for at the moment, and there are differences in people's genes that we don't fully understand. Plus, we don't know all the details of the chemical reactions happening in our bodies.
However, one thing is clear: what we eat has a big effect on these lipid measurements. But, we're not doing a good job of considering this. We tell people to avoid eating before a test, but we don't say for how long. Some people are told to fast for hours, others for days. Some doctors even say fasting doesn't matter. Also, the test results often warn that eating a lot of fat the day before the test can change the results, but we often forget this when we look at the results. Plus, it's not just about what you ate the day before, but what you've eaten over the last few days. And this will affect different people in different ways. Until we figure all this out, these tests aren't that useful.
There's a lot of discussion about whether high levels of a specific type of cholesterol, called LDL-P, is always a bad thing. We don't know for sure yet. For example, a guy named Peter says that high LDL-P can predict heart disease, but I think this is just a connection, not a cause. Peter also agrees that high LDL-P alone doesn't cause heart disease; there are other factors too. So, shouldn't we focus on everything, not just LDL? Peter thinks we should, but says that we don't have good tests for these other factors yet. He also admits that having too little LDL can cause other problems.
Despite all this debate, one thing remains true: eating a high-fat diet and fasting often causes a big increase in LDL levels for many people. Both of which I do on the regular, and which unsurprisingly have given me a high LDL reading, which doesn't bother me at all. The doctor tried to prescribe me a statin, but I told him I'm on keto and no thanks. His reply? "Oh, that makes sense".
Thyroid Stimulating Hormone (TSH)
Missing tests: T3, T4, rt3, and testosterone
Thyroid Stimulating Hormone (TSH) is crucial in controlling the hormone production of the thyroid gland. Elevated TSH levels may signify an underactive thyroid, which could result in symptoms like tiredness and weight gain. Conversely, reduced levels may point to an overactive thyroid, potentially leading to mood fluctuations and sleep disturbances. Consuming foods rich in B vitamins can significantly contribute to maintaining optimal thyroid function.
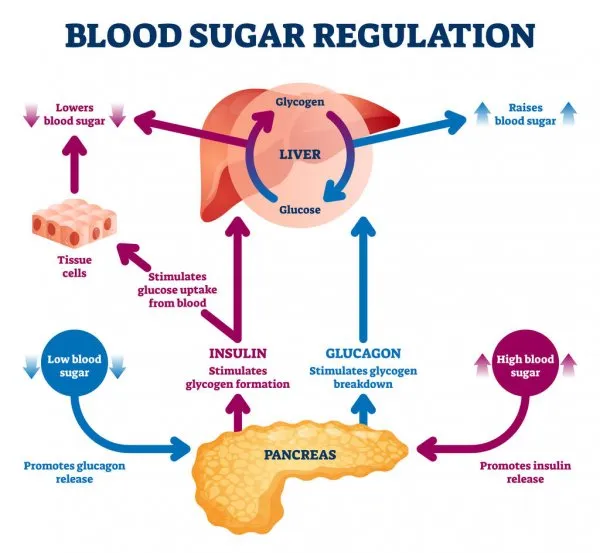
The pituitary gland makes thyroid-stimulating hormone (TSH). TSH tells your thyroid how much thyroid hormone it needs to make. If the thyroid hormone levels in your blood are too low, your pituitary gland makes larger amounts of TSH to tell your thyroid to work harder. Hormones play a large part in many of our daily functions as well as critical life milestones. Hormones affect everything from blood sugar to blood pressure, growth and fertility, sex drive, metabolism, and even sleep. Their influence goes as far as changing the way we think and act day to day.
My levels are pretty high even though they still land in the normal range. Optimally we'd be looking to land somewhere in the middle, as too high levels of TSH have been linked to a lot of problems as well. Problems are similar to Hashimoto's. You want to land in a healthy range, as studies show that metabolic health and good metabolism are achieved in the 1.5 - 2.5 range. When supplementing with iodine you can expect increased TSH levels during your healing. Make sure you're taking cofactors too. Loading iodine on top of a nutrient-dense diet is a great idea before a dry fast so that your body can utilize them where needed during deconstruction and reconstruction.
Iodine and Thyroid stimulating hormone
Iodine supplementation (lugol's iodine) will raise your TSH. TSH is actually a pituitary gland marker, and very often if you have high TSH the doctor will tell you that you have hypothyroidism. This is not always the case. Loading with iodine will increase TSH and it does not always affect you negatively. However high TSH often indicates that you have low levels of thyroxine and the pituitary gland is trying to signal the thyroid to create more. If you want to see thyroid health you want to look for free t3 and t4 levels.
The pituitary gland monitors the level of thyroxine in the blood and emits thyroid-stimulating hormone in greater or lesser amounts if the thyroxine level is too low or too high. The thyroid, physically located separate from the pituitary, then produces thyroxine depending on the TSH level it senses.
In iodine-sufficient individuals, excess iodine intake is most commonly associated with elevated blood concentrations of thyroid stimulating hormone (TSH) that inhibit thyroid hormone production, leading to hypothyroidism and goiter. However, this is not always the case. Sometimes thyroid issues can be resolved with iodine along with its cofactors: Selenium, Magnesium, Vitamin C, and Zinc. Don't overdo selenium. Make sure you're getting magnesium too. Good solution? Eat a few Brazil nuts a day. The key to making sure you're supplementing correctly is to have good stomach acid. It all comes down to absorption. Stomach acid, leaky gut, villi length. All of this can be improved with dry fasting the quickest and most efficiently.
- ½ tsp Natural Celtic Salt, Himalayan Pink Salt, Redmonds Salt or Hawaiin black salt
- 200mcg selenium (L-selenomethionine or Methylselenocystine preferred
- 400 mg Magnesium - Glycinate preferred
- 2,000mg Vitamin C - Ester-C preferred
- ATP Cofactors caplet contains both 100mg B2 & 500mg B3 (Niacinimide) non-flushing in the correct ratio. Take 1/2 caplet with iodine up to 25mg, then one caplet for each 50 mg iodine.
*A.Greens = most cofactors methylated - add salt, and iodine, and mag
*Titrate slowly up to 25-50mg (10-20 drops of lugol's 2%), but start with 1-2 drops daily for a few weeks
Pineal Gland and Iodine
If you feel that your hormones are out of balance, and maybe you have a hard time burning fat and using energy from food, you may have a calcified pineal gland. There is a link between the pineal and pituitary glands. This is due to many things and many toxins in your diet and environment. One of the best ways to work through this is by doing an iodine protocol-focused pineal gland cleanse. Fluoride interferes with iodine metabolism. Iodine chelates fluoride and heavy metals such as mercury, lead, cadmium, and aluminum. Supplementing with iodine can go a long way to detoxifying your pineal gland. Lugol’s 5% iodine solution is a good one to take. But do your research and see what works best for you. Seaweed and kelp are high in iodine content and are easy to add to your diet. If you consider doing high-dose iodine look up the iodine protocol. I may also do a write-up about it in the future. Don't forget 1 tbsp of apple cider vinegar daily for a month.
Unlike the rest of your brain, your pineal gland is not separated from the rest of the body by the blood-brain barrier. It actually has one of the richest supplies of blood, so it is not protected from toxins that can build up in the body over time. Therefore, your pineal gland has the potential to clog, or calcify. Fluoridated water is one of the main causes of pineal gland calcification. When your pineal gland calcifies, you are potentially at risk for a host of health concerns, including neurological diseases such as autism, depression, dementia, anxiety disorder, and Parkinson’s disease. The common thread is that all of these diseases are associated with abnormal sleep patterns, which are directly linked to pineal gland dysfunction.
Adrenal Fatigue and the Thyroid
The adrenal glands, located at the top of each kidney, produce hormones that help the body control blood sugar, burn protein and fat, react to stressors like a major illness or injury, and regulate blood pressure. Two of the most important adrenal hormones are cortisol and aldosterone. When your adrenals are constantly stressed, this sets off an autoimmune, inflammatory response in your entire body. The adrenal-hypothalamus-pituitary feedback loop regulates the secretion of cortisol. All of your organs and your immunity are impacted negatively by the resulting constant assault of cortisol. Low adrenal function can actually cause someone’s thyroid problem to be much worse than it would be otherwise.
Final Notes
Everyone will have different results when taking a blood test. Usually, it can give you indications of what is happening in your body. However, the best indicator is always going to be you and how you feel. There's a reason people feel spectacular a few weeks after a dry fast. Your body starts to run more smoothly.
Seeing near-perfect results on kidney filtration, and liver health is proof that dry fasting does not damage your body the way we've been taught in school and society. In fact, we haven't really been taught anything about it at all. We've just been told Drink water or you'll die. With these results, it's clear that there's more to it than that. It's clear that metabolic water exists, that the body is amazing at self-regulating, and that dry fasting activates deep-level healing. There are studies out there for dry fasting between 3-5 days showing similar results. Actually, all the studies analyzing blood markers show great improvements after a dry fast. Of course, with great power comes great responsibility, and dry fasting should always be approached carefully and responsibly. As long as you follow careful steps for preparation, don't do strenuous exercise during a dry fast, and refeed properly, you will begin a trajectory of healing your body.
Hopefully, you can use some of the discussion here to better understand your own numbers after your dry fast. If you have the opportunity to take blood tests, find a doctor that will requisition them, or go yourself. If that's not an option, then just dry fast, as it's the most cost-effective method of improving your health. The beauty is that as long as you eat a nutrient-dense, whole-food, healthy diet in between fasts, and refeed correctly, you will improve.